
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Summary At Groote Schuur Hospital, head injured patients are managed by the Neurosurgical Department. A retrospective study was undertaken to determine whether the intensive management of head injuries with a low Glasgow Coma Scale (GCS) on admission is justiFied. One hundred and five patients admitted during 1990 with a GCS of 8/15 or less were grouped on the basis of their GCS following resuscitation. Thirty four patients were admitted with a GCS oF 3/15 and fifty two patients were admitted with GCS of 6/15-8/15. The outcome of these patients was then analyzed; the findings suggesting that those patients who have been adequately resuscitated, and have had an intracranical haematoma evacuated, but still present with a GCS 5/15 or less at 6 hours post injury have such a poor prognosis that high tech intensive care may not be justified. Resume Au Groote Schuur Hospital, les traumatises craniens sont pris en charge par le Department de Neurochirurgie. Une etude retrospective a ete entreprise pour savoir si les soins intensifs etaient justifies pour les patients qui a leur admission, presentaient un faible niveau de « Glasgow Coma Scale » (GCS); 105 patients hospitalises en 1990 avec un GCS egal ou inferiur a 8/15, etaient groupes en se basant sur leur GCS apres reanimation; 34 avaient un GCS de 3/15, 7 de 4/15, 12 de 5/15, et 52 de 6/15 a 8/15. Le devenir de ces patients a ete analyse. II en resulte que les patients qui, malgre une reanimation correcte et une evacuation de leur hematome intra-cranien, avaient encore six heures apres le traumatisme, un GCS egal ou inferieur a 5/15, le pronostic etait tellement mauvais que la pratique des soins intensifs de haute technicite ne semblait pas justifiee. Keywords : Severe head injury, Outcome, Glasgow Coma Scale, computerized Tomography INTRODUCTION The management of patients with severe head injuries continues to be a major neurosurgical challenge. With improved monitoring and more effective therapeutic modalities the mortality has decreased but the long term morbidity remains very high. 1,4,9,13 This is even more so in third world countries where there are severe financial and logistical constraints on therapeutic 13 Accurate prediction of outcome would enable the medical team to counsel the family, and to make clinical and legal decisions on a sound basis.5 Numerous studies have attempted to predict outcome of severe head injuries at an early stage2,3,6J,8,10,ll,12,15,16,18,19,21 possible factors in prediction that appear to be of importance include age, clinical coma scales, computer tomography findings, electrophysiological responses and cerebral blood flow. At Groote Schuur Hospital all head injuries requiring admission are managed by the neurosurgical department. Our current policy is that all head injuries receive intensive management, despite the fact that with an increasing patient load the available intensive care resources remain limited. The aim of this study was to determine whether high cost intensive management of all severe head injured patients is justified in terms of the ultimate outcome. PATIENTS AND METHODS In 1990, 105 patients admitted to Groote Schuur Hospital following a head injury had Glasgow Coma Scale values of less than 8/15 after resuscitation. All patients received the following treatment – resuscitation on admission; a CT scan of the head; management in an intensive care unit which included intubation, ventilation, pC02 control, regular electrolyte assessment and sedation. The Glasgow Outcome Scale 14 was used to evaluate the outcome at follow-up. The result was described as favourable if there was a moderate disability or good outcome. An unfavourable outcome was recorded if there was death; a persistent vegetative state or severe disability. The mean period of follow up was 6 months. RESULTS The study showed a preponderance of young male trauma patients with 87% of the patients being male, and 65% being under 35 years of age. The most common aetiology was pedestrian motor vehicle accident (33%); followed by blunt assault (22%); driver or passenger motor vehicle accident (15%) and sharp assault or missile injury (8%) each. 44% of the patients suffered an associated injury, most commonly ormopaeciic in nature, 11% of the patients sustained multiple trauma, having 3 or more injuries and 6% had evidence of hypovolaemic shock on admission. The results of the different GCS groups were then analyzed. Thirty-four patients had a GCS of 3/15 after resuscitation. Thirteen of these patients had head injuries of such severity that they died prior to CT scan being obtained. Of the 19 patients on whom a CT scan was done, 10 showed features in keeping with a diffuse cerebral injury. Four had an isolated intracranial haematoma – either a subdural or extradural haematoma. Three patients had knife tracts and two patients gunshot injuries. 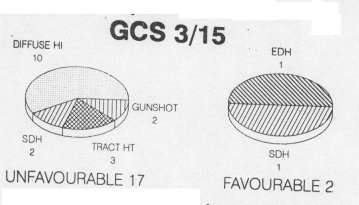 Figure 1 There were 7 patients in the GCS 4/15 group and 5 were investigated. One patient had an angiogram which showed cerebral circulatory arrest and four had a CT scan. Two of these four had features of diffuse cerebral injury and two had acute subdural haematomas. All of the patients in this group had an unfavourable outcome regardless of whether they had diffuse cerebral injury or an isolated intracranial haematoma. 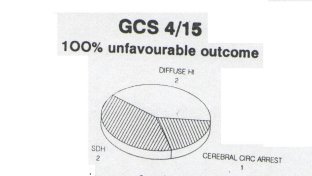 Figure 2 Twelve patients presented with a GCS of 5/15. On Ct scanning six had -features of a diffuse cerebral injury, four had a subdural or extradural haematoma and two had contusions. All the patients with features of a diffuse head injury on CT scan had a unfavourable outcome. However, 66% of patients with an isolated intracranial haematoma had a favourable outcome. 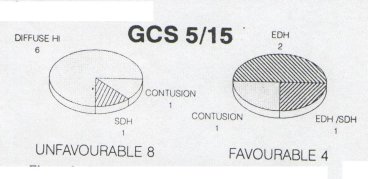 Figure 3 Nineteen patients presented with a GCS of 6/15. On CT scanning twelve showed evidence of diffuse cerebral injury; five had an isolated extradural or subdural haernatoma; one of a knife tract injury and one was normal. Nine of the twelve patients were found to have a good outcome or minor disability. Patients with isolated intracranial haeniatomas had a favourable outcome in 3 out of 5 cases. 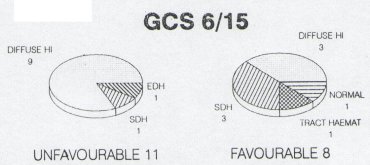 Figure 4 There were 33 patients with a GCS of seven or eight, and thirty-two of these had a CT scan. Findings on the CT scan were eleven subdural haematomas, eight contusions; five extradura. haematonias, seven diffuse cerebral injuries; and one was normal. Five of 7 patients with features of a diffuse cerebral injury on CT scan, either died remained in a persistent vegetative state or had a severe disability. Seventeen of 21 patients with an isolated intracranial haematoma had a favourable outcome. 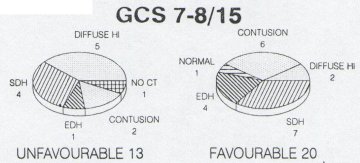 Figure 5 DISCUSSION The aim of most head injury studies has been to determine if there is a group of patients whose injury is so sever that they will not respond to the therapeutic modalities available.l5 If accurate, early prognosis can be made, the available resources can be used to benefit those patients who are more likely to have a favourable outcome.6 The danger which remains, however, is that a patient who may make a significant recovery does not receive optimal therapy. 10,12,16,21 The results of this study suggest that severely head injured patients with a GCS of <5 after resuscitation and with features of diffuse cerebral injury or CT scan have an unfavourable outcome in 100% of cases. If the GCS is >5 there is, however, a favourable outcome in 40%. In patients with isolated intracranial haematornas there is an expected poorer outcome in patients with a lower GCS. Nevertheless, there is a favourable outcome in a significant percentage of patients in GCS groups namely 50% <5 and 71%> 5. Thus there appears to be a group of patients whose head injury is so severe and whose prognosis is so poor, that no intensive management may be justified. They are the patients who once fully resuscitated and on being assessed 6 hrs post injury have a GCS <5 and show no isolated intracranial haematoma on CT scan.
Based on the findings of our study and others in the literature a suggested management protocol to severely head injured patients is illustrated in fig 6.
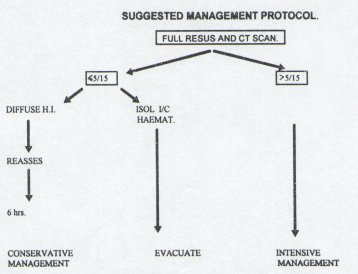 Figure 6 CONCLUSION The authors recognise that this is a small study. It does, however, indicate that based on GCS readings and CT scan performed after resuscitation, there is a group of patients whose head injury is so severe that they will not benefit from intensive management. Limited resources could be more utilised to benefit patients who are more likely to have a favorable outcome.
Summary The author discusses the possibilities of surgery in intractable epilepsies (I.E) in Africa. He has operated 97 cases of I.E. of which great part of them (64 cases or 66 per cent) were post traumatic epilpsies with an exisable scar, 19 cases (19 percent) were mesial temporal sclerosis in whom a temporal lobectomy was performed, seven cases (7 per cent) were cases of infantile spastiz hemiparesis with I.E. and severe behavioural changes treated by hemispherectomy, seven cases (7 per cent) had an anterior callosotomy. No post operative mortality or relevant morbidity has been observed. The best results were obtained in the excision of the scar, hemispherectomies and temporal lobectomies. For the callosotomies a longer period of observation and larger number of cases are needed to have a clear opinion of its effectiveness in the treatment of non focal I.E. Resume L’auteur discute des resultats obtenus par le traitement chirurgical des epilepsies rebelles aux therapeutiques medicamenteuses: 97 patients ont ete operes: 64 fois (66%). L’epilepsie etait d’origine traumatique avec une lesion cicatricielle extirpable; 19 fois (19%) il existait une sclerose temporale pour laquelle une lobectomie fut effectuee; 7 patients (7%) presentaient une hemiparesie spastique infantile avec de graves anomalies du comportement; ces patients ont ete traites par hemispherectomie. Les 7 demiers patients eurent une callosotomie anterieure. II n’y a eu ni mortalite ni morbidite post-operatoire. Les resultats les meilleurs ont ete obtenus dans les cas d’excisions cicatricielles, d’hemispherectomies et de lobectomies temporales. En ce qui concerne les callosotomies, une periode d’observation plus longue et un plus grand nombre de cas sont necessaires pour avoir une opinion valable sur l’efficacite de ce traitement pour les epilepsies non focales. Keywords : Intractable epilepsy, Surgery, Africa Epilepsy is one of the commonest serious neurological conditions in most countries and this undoubtedly true in Africa. Recent epidemiological studies carried out in Kenya (FEKSI et all 1991) shows that the incidence of epilepsy is around two percent, much higher than in the western countries. Studies in four developing countries, Ecuador, Kenya, the Philippines and Pakistan have shown that only a small proportion of patients (8-20%) with active epilepsy are at any one time actually receiving drug treatment. The reason for this failure of treatment are complex, and may involve such no-pharmacological aspects as cultural attitudes to treatment, the acceptability of drugs as a method of treatment, the cost of treatment, and the system for the delivery of health care. In many developing countries there is a shortage of medical manpower and a lack of well organised system of referral, records or health care delivery. The high proportion of untreated epileptic patients may be the cause of the high number of intractable epilepsies seen in the developing countries. The primary therapy for patients suffering for any type of epileptic seizures is medical: anticonvulsive therapy, psychotherapy and social and occupationalrehabilitaion. If the epilepsy is only syptomatic evidence of a progressive lesion of the brain, such as neoplasms, abscesses, haematomas, vascular malformations, congenital or other infective lesions appropriate surgical measures are imperative: we have a large series of these secondary epilepsies but we will not consider them in this paper. In chronic epilepsies, medical treatment should be given a fair trial and considered unsucceessful only when all drugs appropriate to the type of epilepsy have been given alone or in a combination to toxic limits. Such anti-convulsive medication will control the attacks in more than fifty per cent of cases and markedly decrease the seizures in anotlier 25 per cent of cases, thus only 20-25% of the epileptics may become candidates for surgical intervention. The preliminary criteria to be satisfied to consider an epileptic patient for surgical treatment are insufficiency of the pharmacotherapy, the evidence of an organic brain lesion and the handicapping characters of the seizures. Two main groups of surgical approaches are recognised: the first aims at suppressing the seizures by resecting the primary epileptogenic focal area (topectomy, lobectomy, hemispherectorny): the second approach aims only at reducing the epileptogenicity by preventing the diffusion of the epileptic discharges, by enhancing inhibiting or by reducing facilitatory influences (cingulectomy, callosotomy, electrical stimulation of the cerebellum, stereotactic deep lesions and others). In general, surgical procedures that aim to remove epileptogenic tissue together with any identifiable lesion are more common and more successful than those that attempt to modify brain activity. Some neurosurgeons find the subject of epilepsy of no special interest and operations for its relief do not excite them as much as complicated surgical procedures for vascular malformations or particularly difficult tumours. That is not my case: I had my neurosurgical training and worked for fifteen years at the Neurosurgical Institute of the Medical School, University of Padua, Italy, where the surgery of epilepsy was highly advanced, so far that when I left the Institute to start pioneering neurosurgery in Kenya, the Institute of Padua was amongst the highest recognized centres for the treatment of epilepsy. When I started single handed neurosurgery in East Africa in 1967, the load of neurosLirgical work was such that for several years I did little in the field of surgery of chronic intractable epilepsies also because of lack of EEG services, difficulties with neuroradiological investigations and mainly because of other priorities in the neurosurgical field. With improved EEG services and neuroimaging facilities later on my interest in the surgery of epilepsy revived. At the present time, we are sing only two surgical approaches to the treatment of medically intractable epilepsy. One is the older approach of resection of an epileptic focus, and the other is a newer procedure of division of all or a portion of the corpus callosum (Callosotomy). Several other procedures mentioned before and enjoying popularity in the past, including cyngulectomy, cerebellar stimulation, streotactic subcortial lesions and others have now been abandoned. Of the two surgical options in common use now, resection of the epileptic focus has a much higher probability of completely controlling the seizures, thus, the initial evaluation of patients with medically intractable epilepsy should be directed at establishing whether they are candidates for resective surgery. For the selection of patients for resective surgery we follow the classic criteria enumerated by the Montreal School. A focus of origin of the seizures must be identified, and that focus must be in an area of brain where the resection is not likely to lead to an unacceptable neurological deficit: resection is not advisable in the sensorimotor area if a hemiparesis is not already present, or in areas essential for speech or recent memory. The basic lines of inquiries used in our clinic are the following: accurate clinical history and neuropyschological examination (patients should be asked clinical features of their attacks, which will give a clue to the origin; should be asked about interictal events, about past medical history, which may reveal an event sufficient to cause brain damage (as for localized head injuries) and hence the seizures. Other clinical details such as family, developmental, educational and psychiatric history should be investigated – The neurological examination is often negative. EEG examinations: serial EEG is obtained to localize a cortical epileptogenic area if possible. Recordings during drowsiness and sleep (or activation) and sphenoidal electrodes placements are frequently useful. Brain imaging: Computed tomography (CT) scanning makes the detection of small discrete lesions more likely. The CTScans following contrast enhancement of the cerebro spinal fluid with metrizanide may be useful to detect some lesions at the level of the temporal lobe of the lateral ventricles. The magnetic resonance imaging (MRI) detect even greater proportions of such lesions, and is essential in the surgical treatment of epilepsy. The greatest number of intractable epilepsies operated in Kenya are partial post traumatic epilepsies. In the aetiology of partial epilepsy there is a great number of head injuries, particularly depressed skull fractures, unduly common in East Africa. These localized trauma are caused mainly by road traffic accidents and also very common by assaults with a paiiga (a sort of machete in large use mainly in the rural areas) or other sticks. These depressed skull fractures are often incorrectly treated in the peripheral hospitals of the country, laeding to a meningo-cerebral scar that is highly epileptogenic, leading often to an intractable epilepsy. I will recall here the case of a taxi driver involved in an assault in which he had a bad left frontal depressed skull fracture for which he was surgically treated. Seven months later he became a post-traumatic epileptic and his epilepsy became intractable: he could not work and he and his family were facing misery. He came to see me and after all the routine investigations, we excised the left frontal brain scar. As a result of this, he has had no more epileptic fits since 8 years, back happily to his job of driving taxis and I use him often if I need a taxi. Examples as this one are plenty in East Africa and in the whole of Africa and I see no reason and no particular difficulty in treating this type of epilepsies also without sophisticated equipment. We have operated 64 cases of focal post traumatic intractable epilepsy with good results and in over fifty per cent of cases the treatment has been stopped, and acceptable results in the other where the epilepsy is well controlled on medical treatment. In the aetiology of partial epilepsy there is also a relatively high number of patients with either a history of birth trauma, again very frequent in East Africa, or infective or congenital neurological damage. It is often impossible in retrospect to distinguish which of this factors is responsible for the neurological damage but perhaps there is a higher incidence of birth trauma in Africa because of inadequate obstetric services. We have found 19 cases of mesial temporal sclerosis with intractable epilepsy in whom we performed a temporal lobectomy with considerable clinical and EEG improvement in all cases. In seven cases of infantile hemiplegia with pharmacoresistant epilepsy and severe behavioral changes we performed a hemispherectomy with good results in the control of the seizures and a considerable improvement of the behaviour. Since a few years, we have adopted the callosotorny in the non focal intractable epilepsy: the indications were intractable epilepsies associated with injuries and usually characterized by drop attacks of the tonic or atonic types often accompanied by generalized tonic clonic convulsions in patients in whom there was no evidence for well defined removable epileptogenic focus after standard EEG and CT Scan investigations. We usually perform, and anterior callosotomy of 4-6 cm depending on the gravity of the symptoms. We have operated 7 cases with important reduction on the drop attacks, a certain improvement of the control of the epilepsy with medication. We have observed some transient episodes of mutism and akinesia due most probably to interference with cingulate gyri with disruption of cingulum fibres bilaterally. Our experience is limited but the feeling is that perhaps more patients may benefit from this type of surgery. We have no experience at all in subpial transections. Out of 97 patient operated in Kenya for intractable epilepsy we have had no surgical mortality and no relevant morbidity. Improvement in instrumentation, electrophysiological methods and surgical techniques when combined with more precise selection of patients may be expected to provide more benefits in the future. The rationale for surgical excision in epilepsy, therefore, is based on the concept that the removal of a part of an epileptogenic area is rarely effective, but excision of most of this may lead to progressive disappearance of the seizure tendency. RASMUSSEN emphasised the concept that extensive epieptic activity may interfere with the function of the rest of the brain and that the removal of the epileptogenic focus may improve brain function and that the scar of the surgical excision rarely becomes epileptogenic if scrupulous care is taken to preserve the pial surface at the margins of the excision. In conclusion, even in Tropical Africa, we have today in many centres better tools and surgical experience than when the surgery of epilepsy started with PENFIELD and we can help more and more intractable epileptics in this part of the world. SUBDURAL EMPYEMA IN THE KENYAN AFRICASummary Nine cases of subdural empyema in the Kenyan African are reported. This rare but very serious intracranial infection arises as a complication of meningitis ininfants and as a complication of paranasal sinusitis, otitis or trauma in older children and adults. In two cases with chronic posttraumatic subdural haematoma, the hematoma became infected by haematogenous seeding. It is the Author’s opinion that the treatment has a better outcome by draining the pus via craniotomy rather than burr holes. The operative mortality was of two cases (22.2 percent). Resume Neuf cas d’empyeme subdural observes au Kenya sont rapportes. Ces graves et rares infections intracraniennes resultent principalement de complications des meningites chez le jeune enfant, ainsi que des sinusites, des otites et des traumatismes craniens chez les enfants plus ages ou les adultes. Dans deux cas d’hematomes sousduraux chroniques posttraumatique, l’infection etait d’origine sanguine. D’apres les auteurs, le traitement par drainage du pus est preferable apres une craniotomie plutot que par des trous de trepan. La mortalite operatoire a ete de 2 cas (22,2%). Keywords : Subdural Empyema, Kenya, Africa Subdural empyema (S.E) is a rare intracranial infection that .usually arises as a complication of meningitis in infants and as a complication of paranasal sinusitis, otitis or trauma in older children or adults (FEUERMAN et all). Subdural empyema by analogy with pleural empyema – is an appropriate generally accepted term for the diseases, since it is a collection of pus in preformed space. The first thorough clinico – pathological description of the disease were by KUBIK and ADAMS (1943) and COURVILLE (1944). The (S.E) is one of the most serious intracranial infections, so much that the preantibiotic era subdural empyema was almost universally fatal, and that despite surgical and antibiotic treatment, there is still a mortality of 15-40 per cent and a high morbidity rate in the reported scries. MATERIALS AND METHODS The author has operated only 9 cases of subdural empyema: this is 8.3 per cent of all intracranial infections of surgical interest operated in the same period of time (10% for BEDUSCHI and MAROSSERO 1960). The age breakdown in this series is in Table 1. Table 1: Age of patients with subdural empyema
Out of 9 patients, seven were below forty and of these 3 were babies 10-11 months old. Six of the patients were males and 3 females. The subdural empyema was located in all cases at the convexity. The presenting symptoms in this series were similar to those previously reported – fever, headache, nausea and vomiting, meningitism in the early stages, altered mental status focal neurological deficits, focal or generalised seizures in the late referral. Table 2. Shows the clinical breakdown. Table 2: Clinical presentation of patients with subdural empyema.
The duration from the onset of symptoms until the time of surgery ranged from few days to sixty days. The infectious source of the subdural empyema was related to the age of the patient. In all three babies 10-11 months age the S.E. was secondary to meningitis. one following measles, one other concomitant with otitis media. In the 6 eases over the age of 10 years, 3 were secondary to head injuries, 2 to frontal sinusitis and one to chronic oto mastoiditis. All the cases of this series were in the pre C.T. Scanning era: 6 cases had carotid angiography with typical findings of subdural collection and in three babies two subdural taps and one ventriculography confirmed the diagnosis. PATHOGENESIS The pathogenesis of subdural empyema secondary to paranasal sinusitis, was first delineated in the classic paper by COURVILLE. The direct mechanism of infection of the subdural space is by erosion through the posterior wall ofthe frontal sinus and dura; as in two cases of frontal purulent sinusitis, and one case of chronic oto mastoiditis. The indirect mechanism of infection of the subdural space involves the interconnecting venous system of the extracranial and intracranial spaces. Retrograde spread of septic trombophlebitis occurs from the superficial mucosal veins into the dural venous sinuses, cortical bridging veins and cortical veins because these veins are valveless, and eventually the invasion of the subdural space. Table 3: Presumed source of infection in cases with subdural empyema.
In infants, and young there is a diflerent pathogenetic mechanism. These patients nearly always has meningitis associated with the S.E. as opposed to adults. It has been hypothesized that in this young children a subdural effusion forms secondary to meningitis ( 12 per cent of cases); this effusion subsequently becomes infected forming a subdural empyema. Trauma has an important role in the S.E.; not only the penetrating wounds may be the cause, hut also post operative empyemas. Trauma may infect the subdural space even in closed head injuries when a linear fracture involves the posterior wall of the frontal sinus or the ethmoidal sinuses, where the dura is thin and strictly adherent to the bone, may lacerate the dura putting the subdural space in communication with the sinuses: this happened to one of our cases. In cases following a head injury with the information of a subdural haematoma characterised by progressive headache after a free interval of time a sudden onset of high fever, rapid deterioration of the menial status, epilepsy and severe neurological deficits with signs of meningism indicate that the subdural hematoma has become infected and transformed in a subdural empyema: this happened in two of our cases in which one the infection of the subdural hematoma was probably due to associated chest infection and where a streptococcus was isolated and the second, where the infection of the subdural hematoma was probably due to a gastrointestinal infection and where an Escherichia coli was isolated. Most probably the infections of these subdural hematomas is due to a « locus minoris resistentiae » in patients carrying a concomitant infective disease. Facial infections and rupture of an intracerebral abscess may also be considered in the pathogenesis of the subdural empyema. Hematogenous seeding of the subdural space must be exceptional because only DE GROOD (1951) has reported two cases, one following a parotitis and the other consequent to a lung abscess due to actinomicosis. Following DE GROOD, the infection follows the hematic stream, forms a small cortical abscess that opens in the subdural space. Table 4: Organism in subdural Empyema
In infants the most common organisms found in S.E. is the Hemophilus Influenza and Aerobic Streptococcus as in two of our babies. In 5 other cases the bacteriology showed: Staphylococcus aureus hemolyticus, staphylococcus aureus, anaerobic streptococcus in two cases, bacterium coli in one case. In two cases the pus was sterile. TREATMENT Rapid diagnosis, surgical removal of the irritating pus and appropriate antibiotic therapy are the principles that form the cornerstone for management of subdural empyema. (FEUERMAN et all 1989). The rapid diagnosis of S.E. is not always easy, but when the classic syndrome of headache, nausea, vomiting, fever and meningism followed-by neurological deficits and seizures is present in conjunction with parasanal sinusitis, otitis or mastoiditis, the diagnosis of intracranial suppuration (either sudural empyema or brain abscess) is clear. When no history ofotorhinologic disease is present, the diagnosis is difficult between that from brain abscess, meningitis, cerebritis or viral encephalitis. But in the suspicion of S.E. or brain abscess, mainly in the presence of focal neurological deficit or focal seizures, neuro-radiological investigations (angiography where scanning is not available), C.T. scan with contrast and even better M.R.I, are mandatory. The M.R.I, will help also to identify, in case ofS.E., the possible extension of empyema in the interhemisperic fissure, the opposite side and in the posterior fossa. It has been reported by various authors (BANNISTER et al) that the CT Scan may be normal or not indicative of a subdural empyema. In this cases it is suggested tisal if the clinical evidence is in favour of subdural empyema and considering the gravity of the infection, a surgical exploration is indicated, or else, the use of angiography or better M.R.I. Once the diagnosis is radiologically confirmed immediate surgical drainage should be undertaken. Since the advent of C.T. scan with usually accurate localization of the empyema, selective burr holes with irrigation of the cavity through the burrholes has been advocated (RENAUDIN et al-1980). BANNISTER et al (1981) take exception to this approach in their publication. They reviewed their experience with 66 cases and a further 309 cases that has been reported in the literature by 1980 and reach the conclusion that a better outcome was achieved by draining the pus via craniotomy rather than burrholes. They attributed this improvement to more complete removal of pus, which can be loculated, thick and tenacious. Thus, burr hole drainage, even with catheter irrigation, may not adequately drain an empyema. This recommendation is substantiated by the experience of FEUERMAN et al (1989) and by our modest experience of 3 cases published in 1961 and other nine cases treated in Kenya. Table 5: Type of surgery and outcome in cases of subdural empyema
In our series two cases had burr holes as a first treatment: the first case a subdural empyema was evacuated elsewhere through burr hole: he was later referred to us in coma and a craniotomy was performed but the patient died. The second case a baby had a ventriculography and drainage of a subdural empyema during the procedure, required craniotomy 4 days after with complete recovery. The other 7 cases had all primary craniotomies with one death and one patient recovered (a baby) with severe hemiparesis. In our series of 9 cases there is a mortality of 50% in cases in which the burrhole was the first treatment followed by craniotomy, and a mortality of 14.2% in the case: treated with primary craniotomy. The total mortality rate was of 2 cases over 9 (22.2 percent). The drug of choice before the culture results are hand, and usually afterwards, is chloramphenicol that has been used in all our cases. It penetrates the blood-brain barrier and the brain tissues well (BANNISTER et all -1981). Topical chloramplienicole was used in the first 4 cases: in the last 5 cases topical Rifampicine was used. The dura was closed in 8 cases and left open in one case. A subdural drain was left in all cases but have not been used for irrigation post-operatively. In all cases the bone flap was removed to avoid possible risks of post operative osteitis and also as decompressive measure. In conclusion, an early diagnosis followed by radical removal of pus at the earliest possible stage by a large craniotomy and antibiotic treatment seems to be today the treatment of choice. Articles récents
Commentaires récents
Archives
CatégoriesMéta |
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647





