
|
|
|
Introduction Parkinson’s disease (PD) is a chronic delibitating disease, complicated by cognitive dysfunction and associated with increased caregiver burden, pressure on community health facilities and significant mortality (56,4). Most of the data concerning cognitive dysfunction in PD are based on studies done in Europe and North America. There is paucity of data on cognitive impairments among PD patients in Sub-Saharan Africa. Knowledge of the pattern of cognitive dysfunction and predictive factors peculiar to different geographical regions may be important in early identification of this complication and ensuring appropriate channelling of resources into caring for patients with PD. Cognition referes to all mental activities associated with thinking, knowing, remembering and communicating. It eencompasses problem solving, decision making, mental grouping of objects and forming judgements (46). The major classes of cognition include reception (ability to select, acquire, classify and integrate information), memory and learning (which involve information storage and retrieval), thinking (involving mental organization and recognizing the information), and expressive functions (which involve speaking, drawing, writing, physical gestures, facial expressions and movements) (46). The prevalence of cognitive impairments in PD has been reported in several developed countries. A systematic review of 27 studies by Cummings reported an average prevalence of 40%. while Aarsland et al. found the prevalence of cognitive impairments in PD to range between 24 and 31% (14,1). The UKCamPaIGN study obtained a prevalence of 36%, while Muslimovic et al. found a prevalence of 24% in a cohort of newly diagnosed PD patients in the Netherlands(31,54). One of the few studies from the sub-Saharan Africa by Osuntokun and Bademosi found a frequency of 5% but a more recent study by Akinyemi et al reported a frequency of 21.6% (61,4).
The diagnosis and type of cognitive dysfunction in PD from previous studies were determined with the use of neuropsychological test batteries requiring professionally skilled personnel and were both time consuming and costly. This placed a lot of stress on the patient and administrators of such test batteries. The Six Item Cognitive Test (9,12,16,17,23,43,75), is a very simple test which could be administered by non-professionals in an average time of three to four minutes. It is a reliable test which has not been validated in patients with PD in our environment. The dearth of information on the pattern and predictive factors of cognitive dysfunction in sub-Saharan African region prompted this study. Therefore, this study sought to determine the frequency and pattern of cognitive dysfunction amongst patients with PD presenting at a tertiary health facility in south-south Nigeria and compared the performance of the PD patients with demographically matched subjects without PD (controls). In addition, we assessed the contributory roles of patient and disease variables to the development of cognitive impairments in PD patients. This study alsosought to validate the Six Item Cognitive Impairment Test in patients with PD in a resource limited environment. Materials and methods Study site The study was carried out in the Neurology outpatient’s clinic of a tertiary health facility located in the cosmopolitan south-south Nigeria. The health facility is situated in the capital of Edo State and serves as the main referral centre for the state and four neighbouring states. Study population Patients with PD, without diabetes mellitus or hypertension, presenting for treatment on an out-patient basis at the medical outpatient clinic of the hospital. Patients were examined by one of the authors (MO) and clinical diagnosis was made based on the UK Parkinson’s Disease Society(UKPDS) Brain Bank Clinical Diagnostic Criteria(39). Inclusion Criteria for patients
Exclusion Criteria for patients
Inclusion /Exclusion Criteria for Controls Normal healthy individuals who fulfilled the above inclusion criteria except that they did not have features of PD or Parkinsons Syndrome, were recruited from thehospital staff and general population, and they freely volunteered to be part of the study. They were age, sex and level of education matched with PD patients. Sampling technique Patients with features of PD who met the inclusion criteria were recruited consecutively at presentation in the neurology outpatient clinics. Sample size A total of 30 patients were recruited for the study.The minimum sample size of patients required for the study was 28, calculated based on the Kish method(44). n = z2 pq = 1.962 x 0.0006 x 0.9994 = 28.44 d2(0.009 )2 n = the desired sample size ( when population is greater than 10,000 ) z = the standard normal deviation, usually set at 1.96, which corresponds to the 95% confidence level p = proportion of patients with PD estimated at 59 per 100,000(8,20,21) q = 1- p d% = absolute deviation from p% that will be tolerated ( i.e. p% give or take d% ) Study design Recruited PD patients with age-, sex-, and level of education-matched controlsreceived clinical assessment using standardised questionnaires to document demographic information and disease related variables including primary language used and reading abilities, level of education, medical history and psychiatry history. A detailed neurological examination was performed on all patients to verify the clinical diagnosis of PD. The stage and severity of the disease were determined using the Hoehn and Yahr staging scale and motor subscale from the Unified Parkinson’s Disease Rating Scale(UPDRS) (38,27). The duration of the disease was defined by the period between the onset of the first symptom as reported by the patient and the time of clinical assessment. Cognitive performances of recruited study participants (PD patients and controls) were assessed with the Six item Cognitive Impairment Test(6CIT) (9), and a computer-based cognitive instrument, the Iron Psychology (acronym-FePsy) (73,58). All the questionnaires were in English language as most people in the locality speak English. The 6 CIT tool The Six Item Cognitive Impairment Test is a simple test which can be administered in three to four minutes. The 6CIT was developed in 1983 by regression analysis of the Blessed Information Memory Concentration scale (BIMC)(9,43). It is an abbreviation of the latter. It is brief, simple, easy to perform and can be translated linguistically and culturally. It correlates well with the MMSE and even outperforms it in milder cognitive dysfunction. Since it is less time consuming, it could be suggested that it is superior to the MMSE. It consists of a total of six questions meant to test memory, orientation and concentration. The total duration of the tests is short; about 3-4 minutes. It uses an inverse score and questions are weighted to produce a total out of 28. Scores of 0-7 are considered normal while 8 and above are cognitively impaired. The 6CIT has been validated in several published studies(9,12,16,17,43).An advantage of this test is its high sensitivity without comprising specificity even in mild dementia. The 6CIT has a positive predictive value of 100% and a negative predictive value of 83.33%. The 6CIT has been validated among Nigerian patients with chronic kidney disease(23) but no validation study has been carried out among patients with PD in Nigeria or other West African countries. Astudy for validation of its use was therefore carried out prior to the main study. The name and address “Amen Bazuaye, 10 Lawani Street, Benin” was used as a substitute for the traditional but foreign “John Smith, High Street, Bedford.” The Iron Psychology (FePsy) In 1978 C.H.W. Van Ziji developed the Iron Psychology (Fepsy), which is a system for automated neuropsychological testing. It is a powerful, automated menu-driven neuropsychological computerized test battery (73) that covers arousal, short term memory, mental speed and vigilance. It contains a set of computerized tests for cognitive functions and a relational database system for storage of the results; each subject undergoes computerized testing to assess cognition (59,5). These test items include: (1) Simple reaction time tasks (auditory reaction time and visual reaction time) which assess mental speed. (2) Binary choice task assesses complex mental speed and concentration. (3) Recognition tasks (simultaneous recognition of words, simultaneous recognition of figures, serial recognition of words, serial recognition of figures) which test for memory. (4) Tapping task which tests motor speed. (5) Vigilance task: this task assesses attention. (6) Corsi’s and Binnie’s Block tapping task: for abstraction, concentration and attention. (7) Computerized visual scanning task (CVST): for assessment of brain damage, abstraction, attention, concentration and mental speed. (8) Rhythm task: this tests memory. (9) Classification task: tests for abstraction. (10) Visual half field tasks: this assesses concentration and includes recognition of words, recognition of figures, matching of lateral words and matching of central words (19,22,35,68). Ethical consideration Ethical approval was obtained from the institutional Ethics and Research Committee before proceeding with the study. Informed written consent was obtained from patients and controls or a reliable relation before recruitment after proper explanation of the study procedure. Recruited study participants were compensated with transport allowance. Statistical analysis Data were analyzed using the Statistical Package for Social Sciences version 16.0 (SPSS) (70).Demographic characteristics of cases and controls were compared using the Student’s t-test for continous variables, while categorical parameters were analyzed using Chi-squared test. Clinical characteristics of cases were summarized using the mean and standard deviation (SD). Cognitive performances of cases and controls were compared using the Student’s t-test, whereas independent predictors of cognitive dysfunction were identified using odds ratios (ORs) from logistic regression models. The confidence interval was set at 95% and a p-value of 0.05 or less was considered statistically significant. RESULTS Determination of cut-off score on the cognitive tool and validation assessment The mean age for the patients was 50.9 (SD 18.59) years, while that of the controls was 51.5 (SD 12.26) years, with no significant difference (t=0.0908; p=0.929). The patients comprised 5 males (50%) and 5 females (50%), likewise the controls. The level of education distribution for both groups were also same: 2 with primary education (20%), 4 with secondary (40%) and 4 with tertiary education (40%). The mean total error scores for the controls and patients were 1.67 (SD 2.06; range 0-6) and 13.7 (SD 8.47; range 4-28) respectively, with a statistically significant difference (t=4.364; p=0.0004) using the 6CIT. By implication, the total correct score followed the reverse pattern with mean scores of 26.33 (SD 2.06; range 22-28) and 14.3 (SD 8.47; range 0-24). The receiver operating characteristic curve (Figure I) was obtained for the total error scores to determine the cut-off score that corresponds to the optimal sensitivity and specificity values for the 6-item cognitive tool. The optimal cut-off score of 6 was obtained with a sensitivity of 71.43% and specificity of 96.43%. The accuracy of the 6CIT tool was 83.93%. This cut-off score was same as that obtained by Katzmanet al.9 The area under the curve (AUC) of 0.85 (SE 0.575) was significant with 95% confidence interval at 0.7373 – 0.9629). The cut-off error score of 6 was used for this study. Results of main study Demographic data of patients and controls. Thirty PD patients and age-, gender- and educationally matched 30 controls participated in the study. The means of their ages were 69.10 ± 7.47and 68.73 ± 7.06 years respectively with male preponderance. The demographic data of the PD cases and the controls are summarised in Table III. *Fisher’s Exact Test The male : female ratio was 26 : 4 for both the PD patients and the controls. This is shown in figureII. The mean age for the PD patients was 69.10 ± 7.47 years, while that of the control was 68.73 ± 7.06 years (p=0.846). The highest freguency of 8 (26.7%) was found in those aged 64-68 years, while the least, 3 (10%) each were in those aged 54-58 years and 79-83 years. This corresponded with that of the control with a p value of >0.05 which was not statistically significant. The proportion of patients and corresponding controls in the stratified age groups is shown in Figure III. The level of education of the PD patients ranged from nil formal education (10%) to tertiary level of education (36.7%). Those with primary level of education were about 20% of the studied population while those with secondary level of education constituted 33.3%. This corresponded with that of the control with a p value of >0.05 which was not statistically significant. Figure IV is a graphical representation of the distribution. Clinical characteristics of the patients with PD The highest proportion of PD cases was seen in stages 2 and 3 of the H and Y scale, each comprising 12 (40%) subjects. The lowest proportion was in stage 1 with 1 (3.3%) patient, while stage 4 had 5 (16.7%) patients. Figure V reflects the stages of PD in the population studied. The overall UPDRS score range for the PD patients was 7 – 64, with a mean of 35.23 ± 14.69. The scores for the males ranged between 7 and 64 with a mean of 35.15 ± 14.25, while those of the females were higher ranging between 22 and 64 with a mean of 35.75 ± 19.81. Table IV reflects the UPDRS rating of the PD patients. Cognitive performance among patients with PD and control subjects on FePsy The patients with PD performed poorly in all cognitive domains of FePsy except the binary choice reaction time and non-dominant hand on finger tapping when compared with the controls. The results of their performances are presented in Table V. The performance of the PD patients on 6CIT was significantly affected by age group (p=0.014), being worse with increasing age, and the UPDRS score being worse with higher scores. However, performance was not significantly affected by H&Y stage, nor disease duration with P values > 0.005. The result is presented in Table IX . PD cases with higher UPDRS scores were impaired with higher scores on the 6CIT being an inverse scoring system with a p value of 0.001 which was statistically significant. The box plot in Fig XI shows the relationship between patients performance on 6CIT and their UPDRS score. The PD patients with longer disease duration were impaired on the 6CIT, however this was not statistically significant at a p value of 0.205. This relationship is shown in Figure XII. The poor performance of PD patients on 6CIT corresponded with lower scores on apraxia. This was significant with a p value of 0.049. This is shown in Figure XIII. The PD patients had worse performance on 6CIT with increasing age. However, this was not significant statistically at a p value of 0.194. This is shown in Figure XIV. Performance on the 6CIT was worse for the PD patients compared with controls, however this was not statistically significant at a p value of 0.114. This is represented in Figure XV. Discussion Demographic data of the patients with PD Thirty PD patients participated in this study. The patients were age-, gender-, and educationally- matched with controls to allow unbiased comparison of results. The mean age of the patients was 69.10 ± 7.47 years with a range of 64-78 years. This may be due to the fact that PD is rare before the age of 50 years with a sharp increase in incidence after the age of 60 years (18,26). Majority of the patients that presented during this period were males and this is consistent with earlier studies that have reported a higher prevalence of PD in men than in women (8,13,28,50,53,57,60). The Hoehn and Yahr staging of the patients ranged from 1 to 4 with most patients in stages 2 and 3. This may be due to the fact that most patients with PD do not present early probably due to lack of impairment in activities of daily living in the early stage of the disease and in the late stage a number might have died either from complications of the disease or other age related illnesses hence the majority of patients were within the middle stages of 2 and 3. Frequency of cognitive impairment in PD The PD cohort studied had significant cognitive impairment as demonstrated in their performances on all the neuropsychological tests used. This is similar to findings in previous studies on cognitive impairment in PD. The frequency of cognitive dysfunction in the PD patients was 53.3% using the 6CIT. This is higher than those obtained in other studies, Cummingsobtained an average prevalence of PD dementia of 40% in a review of 27 studies, while Aarsland et al. in a systematic review found the prevalence of PD to range between 24-31% (14,1). The UK CamPaIGN study obtained a prevalence of 36%, while Muslimovic et al. found a prevalence of 24% in a cohort of newly diagnosed PD subjects in Netherlands (31,54). Osuntokun and Bademosi found a frequency of 5% in a study in Ibadan, however Akinyemi et al had a frequency of 21.6% (61,4). The variation in prevalence of PD from these studies may be attributed to differences in methods of cognitive assessment, operative definition and the study population (24). This study was however on cognitive impairment and not just dementia alone. Pattern of cognitive impairment in PD The 6CIT assessed memory alongside attention and concentration, and orientation. The computer based neuropsychological tool Fepsy assessed memory, reaction time and motor speed. The overall performance of patients with PD on the test instruments was significantly worse when compared with the performance of the healthy subjects. The patients overall performance in the memory cognitive domain was poor compared with the controls. Memory deficit in PD is more a problem of retrieval of coded information than a deficit of registration, encoding and storage of information (56,48,66). This was demonstrated in this study by the performance of the PD subjects in the address registration, recall, and overall memory score. Their performance was worse than that of the controls. Language deficits have been well described in PD and these include naming difficulties, decreased information content of spontaneous speech, impaired comprehension of complex sentences, as well as verbal fluency (7,63). These were exhibited in our cohort of subjects. Confrontational naming defects exhibited by our subjects may be as a result of direct neuronal degeneration associated with hippocampal and limbic deposition of Lewy body pathology in PD (11). However, in many described language deficits, the anatomical regions of the brain responsible for language function are not primarily affected by the disease process, rather they may be related to the dysequilibrium syndrome that characterises PD (25,69). In addition, patients with PD may develope a limbic or hippocampal type of amnesia similar to that seen in Alzheimer’s disease. Such subjects are those in whom AD and PD co-exist or those with AD type pathology (15). The patients with PD performed worse than the controls in the tests assessing executive dysfunction such as the comprehension-motor response. The timed test offers some quantitative measure of the speed of cognitive processing (reduced in PD). PD patients are impaired in tasks requiring the spontaneous elaboration, maintainance and change of cognitive strategies (10,30,36,52,71,76). The dorsolateral pre-frontal cortex has a crucial role in self-directed planning of behaviour and is central to frontal/executive functioning. It’s dysfunction in PD has been alternatively attributed to the disruption of the ‘‘Complex Loop’’ linking pre-frontal to basal ganglia or damage to the ascending dopaminergic mesocorticolimbic pathway (71,41). Some authors however have emphasised the possible role of non-dopaminergic lesions involving cholinergic and noradrenergic systems (65,64,32). Hence, cognitive dysfunction in PD may result from multiple neurotransmitter deficits including dopaminergic, cholinergic, serotoninergic, and noradrenergic systems (25,3,49). According to Fanna et al (29), the dysfunction of the “Complex Loop” would be combined with damage to the “Motor Loop”, a functional anatomic circuit connecting the putamen to the supplementary motor area, whose disruption would be responsible for the motor disability. However, another hypothesis attributed the frontal-like neuropsychological abnormalities observed in PD to the loss of dopaminergic neurons in the ventotegmental area; affecting meso-cortico-limbic pathways, causing dopamine depletion in various cortical areas, including the pre-frontal cortex (45,74,67). The IronPsychology (FePsy) was also used in the evaluation of cognition of both patients and controls. This test has been validated in Nigerians which therefore justifiesits use (46). The subsets of FePsy used in the study included the simple reaction time (auditory and visual), the binary choice reaction time, the recognition memory test and finger tapping task. Subtle subcortical cognitive impairments can be detected by the timed tasks characterized by general slowing of psychomotor speed and thought processes. The reaction times for both patients and controls were found to be much higher than the normative values. In the normative study, a desktop with the keyboard resting on the person’s laps was used while in this study; a laptop with component keyboard resting on the table was used. In the latter case, the reaction times were expected to be more prolonged due to the ‘hand – reaching effect.’ This may also have caused a disparity in the word score between the control subjects in this study and the normative subjects. The PD patients performed worse than controls in all cognitive tasks except in the binary choice reaction time where there was no difference, even though the binary choice sensitivity was less in them.There was also no difference in the tapping task involving the non- dominant hand compared with the control. Therefore, patients with PD may be at higher risk of memory impairment and may have general slowing of psychomotor speed and thought processes. However, their concentration abilities may not differ from the general population.Information processing speed refers to the brain’s ability to rapidly process simple and complex information. Activities of daily living require constant information processing, impairment in psychomotor speed and thought processes as demonstrated by the patients could explain the dysexecutive syndrome seen in these patients. The 6CIT assessed the cognitive domains of memory, concentration and orientation ( in time). The patients demonstrated impairment in all three domains tested. Concentration is the ability to focus and sustain attention, while attention is a cognitive function of the brain that enables a person to triage relevant inputs, thoughts and actions while ignoring those that distract or are irrelevant. Attentional deficits were described as an independent risk factor by Taylor et al (72). Memory deficits in PD have been well described (56,41,66) this was demonstrated with the 6CIT in this cohort of PD patients. Predictors of cognitive dysfunction in PD In this study, certain variables were demonstrated to be predictors of cognitive dysfunction. The age- groups correlated positively with 6CIT and this was related to the level of overall cognitive function. Being an inverse scoring system, it means cognitive function worsened with increasing age groups. The Campaign cohort study revealed that age greater than 72years was an independent predictor of cognitive decline in PD patients (78). Age at onset of the disease and disease duration were not found to be predictors of cognitive dysfunction. This is in keeping with Hughes et al. who found no relationship between age at onset of the disease and cognitive decline (40). Aarsland et al. (2) in another study, showed that it is the general effect of age rather than the age of PD onset that contributes most to the incident dementia in patients with PD, while Lyros et al. (51) showed that the cognitive decline in PD patients might be owing to simultaneous effect of age-related and disease associated neuropathology. This was at variance with Akinyemi et al.(4)who demonstrated that older age at onset of PD showed significant association with cognitive dysfunction. Previous studies have shown that the most important clinical predictors of global cognitive decline following correction for age were neuropsychological tasks with a more posterior cortical basis well as a postural instability gait abnormality (non-tremor dominant) motor phenotype at the baseline assessment (72,78,1,42,79,47,6). This study also demonstrated that recall was significant, however was at variance with the previous studies in that gait abnormality was not found to be a significant predictor of cognitive dysfunction. This study demonstrated that greater severity of PD as indicated by higher Hoehn and Yahr stages or higher scores on the UPDRS motor subscales was associated with worse cognitive profile which was in keeping with previous studies (4,54,55,9). There was no significant relationship between years of formal education and cognitive decline. This is in keeping with studies by Akinyemi et al.(4) and Pai and Chan (62) who also found no significant relationship between the the number of years of formal education and cognitive decline in patients with PD. However Glatt et al.(33)and Green et al. (37) found an association between lower educational attainment and cognitive decline in subjects with PD. Comparison of the test instruments Determination of the nature and degree of cognitive impairment in PD requires comprehensive assessment of cognitive abilities including speed of information processing, attention, memory, language (fluency) and executive functions, which are necessary for goal- directed behaviour. There are a wide variety of such cognitive tests including Cognistat, D2 test of attention, digit vigilance test, Halstead-Reitan neuropsychological battery, Kaplan neurocognitive assessment, Luria-Nebraska neuropsychological battery and the Iron psychology (acronym FePsy), a computerized assisted test battery that contains finger tapping test, auditory reaction time, visual reaction time, visual scanning and binary choice tests. Other neuropsychological tests include Wechsler intelligence scale, trail making tests A and B, Stroop test, tests of memory and learning (TOMAL) and technical performance test (77). The six- item cognitive impairment test (6CIT) (9) and the MMSE are further examples. The 6CIT is sensitive for assessing cortical dementia, however has limited coverage of the cognitive domains. The 6CIT assessed memory (short term), orientation (time) and concentration. In assessing existing tests and test batteries for evaluation of cognition, useful tests are those that are rapid, repeatable, highly reliable, not dependent on experts for administration and free of significant re-test effects (34). This favours the 6CIT, however, a drawback for the 6CIT is its limitation in the range of domains assessed. The timed task tests on Fepsy, a speeded test, are sensitive for detecting subtle subcortical cognitive impairments characterised by generalised slowing of psychomotor speed and thought processes. The generalised slowing of psychomotor speed and thought processes contribute to the dysexecutive syndrome seen in patients with PD. Other domains of cognitive function assessed by FePsy include memory (short term, verbal and non-verbal), abstraction, attention and concentration. Being a computer based instrument, it is subject to less administrative bias the 6CIT. This study assessed cognitive function of PD patients using 2 tools; (a) 6CIT assessed for its utility as a screening tool, (b) FePsy subcortical, thereby covering all the cognitive domains both at the cortical and subcortical levels. The cognitive tests in FePsy are essentially ‘timed’ tasks thus revealing the significant deterioration in mental and motor speed which can not be adequately tested with the 6CIT. CONCLUSION This study showed that there is a high frequency of cognitive impairment amongst patients with PD compared to demographically matched controls and this worsens with the stage of the disease on Hoehn and Yahr staging and with increasing UPDRS score. Other predictors of cognitive impairment in the PD patients included age of the patient and recall. The pattern of cognitive impairment seen in these patients included memory, psychomotor speed, complex mental speed and visuoperceptual dexterity. This study also validated the Six item Cognitive Impairment Test (6CIT) as a screening tool for cognitive dysfunction in patients with PD in the Nigerian population. As a cognitive tool, it is brief and simple, can be translated culturally and linguitsically with good probability statistics. Limitations This is a cross sectional study, as a result it may not capture PD patients with more advanced stage of cognitive impairment. This is a common limitation with this type of study design. The use of the FePsy requires some computer literacy on the part of the investigator. This underscores the relevance of the 6CIT tool which is a non-computer based psychometric test in a resource poor setting. RECOMMENDATIONS All PD patients should be screened for cognitive impairment using neuropsychological tests by their health care providers. Cognitively impaired patients may undergo neurological evaluation with social and vocational adjustment or rehabilitation. Most of these PD patients are dependent on others for means of livelihood due to incapacitation by the disease. There is need for support groups such as the Parkinson’s society. Further studies are recommended to increase knowledge of this disease and the impact on the cognitive function of affected individuals. This will help in the management of these individuals. 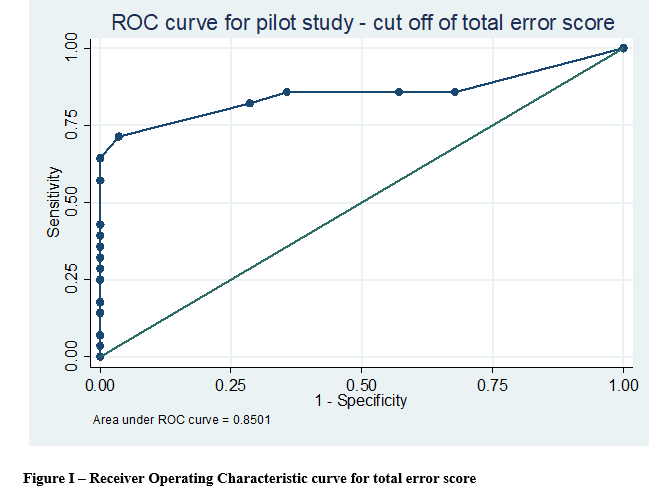 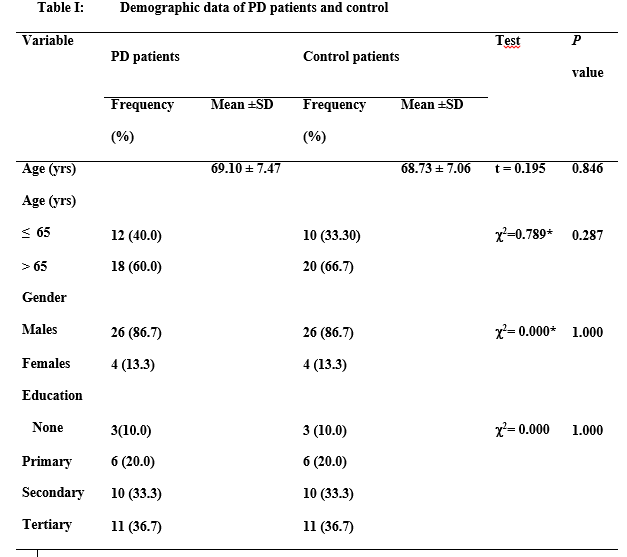 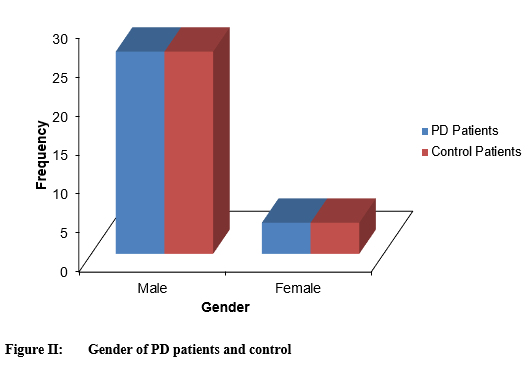 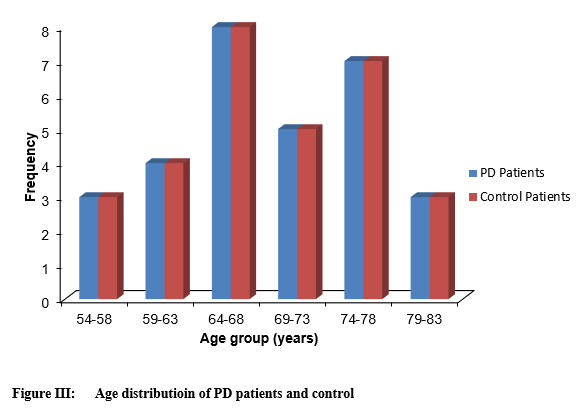 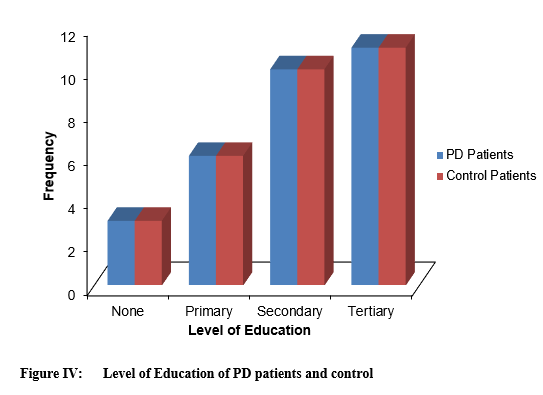 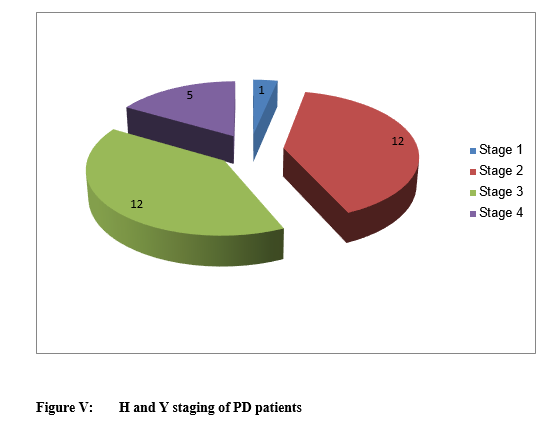 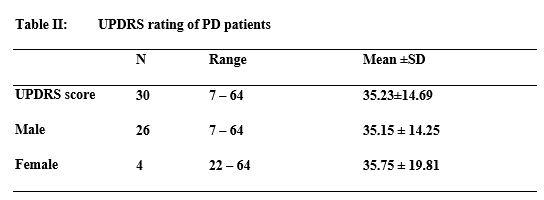 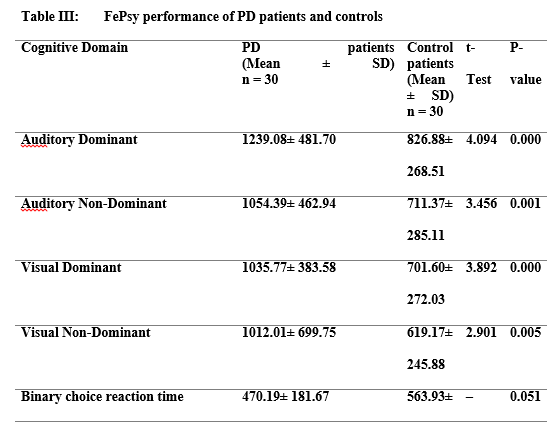 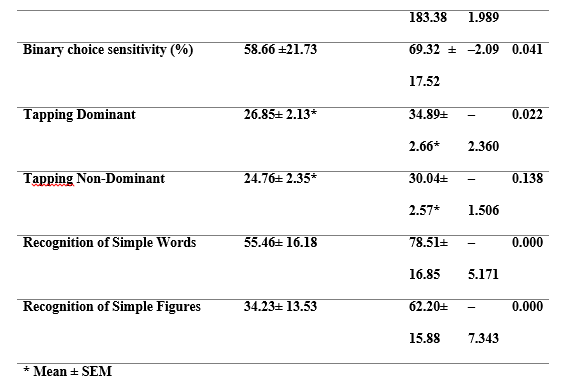 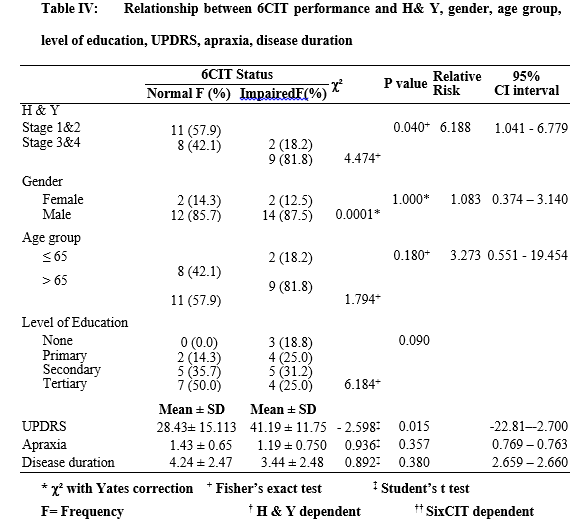 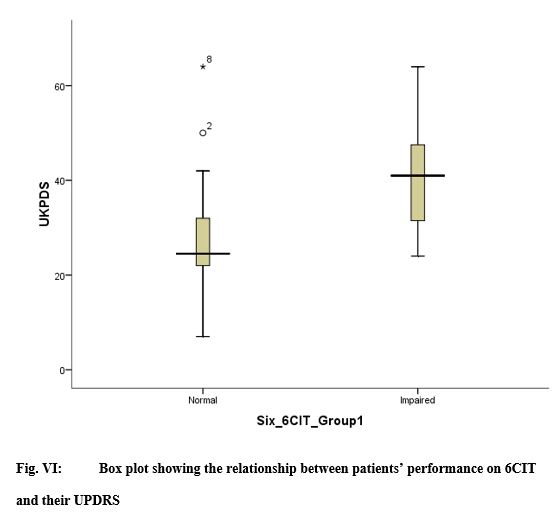 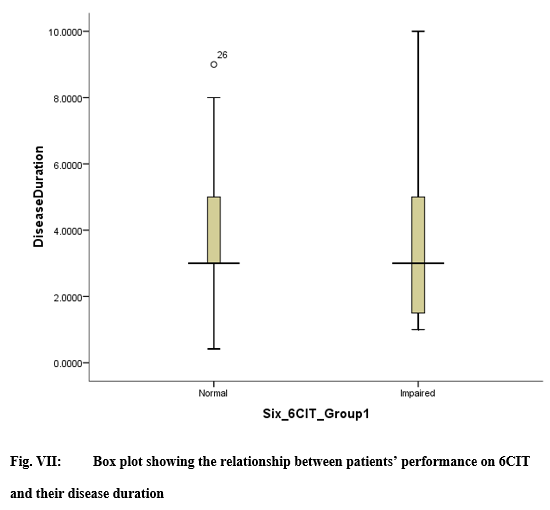 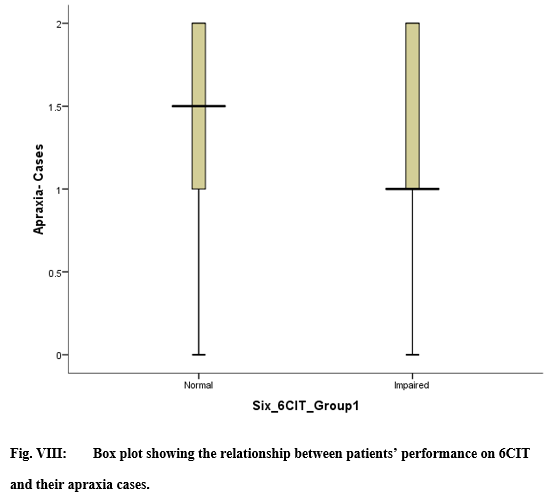 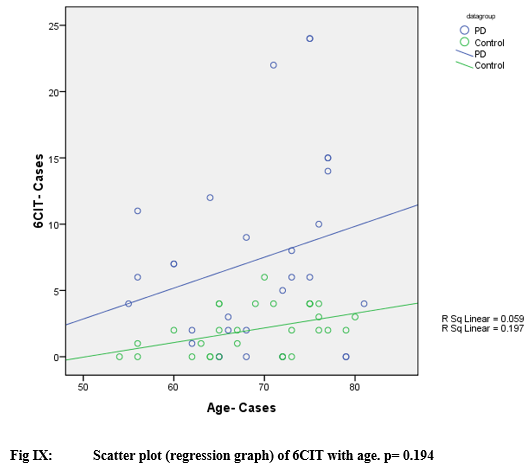 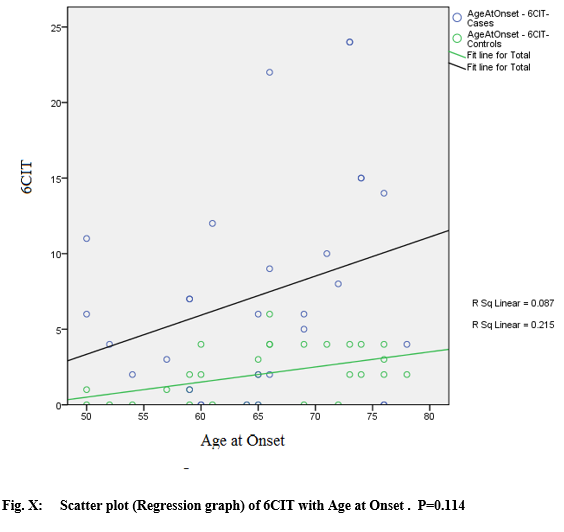 I- INTRODUCTION: From the early 1990s onwards, the management of intracranial aneurysms (ICA) was revolutionised by the advent of endovascular treatment, which has been continuously improved to this day. (13) Despite all the advances in neuroradiology, surgical treatment has retained its place in the management of ICA, with a better rate of complete occlusion. (19; 20; 14) However, there are complications associated with incorrect placement of the clip during surgery, such as a residual collar exposing the patient to the risk of rebleeding, or ischaemia occurring when one or more branches of the carrier vessel are inadvertently caught in the clip’s bites (6; 9). The morbidity and mortality associated with surgical treatment are therefore increased. The occurrence of these complications, despite meticulous microscopic inspection after clip insertion, has led to the development of techniques such as microvascular Doppler and fluorescein angiography to make the operation safer (8). In Senegal, despite the recent advent of embolisation, the treatment of intracranial aneurysms has remained surgical to date, due to a lack of financial resources for the vast majority of patients. Since the acquisition of microsurgical Doppler by our centre, aneurysmal microsurgeries have been systematically monitored by Doppler after clipping. We conducted a retrospective, descriptive and comparative study based on a prospective register of all patients who underwent surgery for the management of an intracranial aneurysm in the neurosurgery department of Fann national teaching hospital between January 2013 and December 2019. The aim of this study is to establish the impact of intraoperative use of microvascular doppler on outcomes of intracranial aneurysm surgery. II- METHODS II-a Design, setting and period of study: We conducted a retrospective, descriptive and comparative study based on a prospective register of all cases of intracranial aneurysms treated surgically in the neurosurgery department of Fann national university hospital. Based on a prospective register of all patients treated for neurovascular pathologies in the department, we carried out a retrospective selection of patients treated for intracranial aneurysms. We included in this study all patients who underwent surgery for the exclusion of an intracranial aneurysm during the period from January 2013 to December 2019, and whose medical records were complete and usable. II-b Parameters of interest, outcome and operational definitions: The parameters studied covered the following aspects: Epidemiological aspects (age, sex, risk factors, history, etc.). Clinical aspects (time to hospitalisation, length of hospitalisation, classification according to the WFNS clinical severity scale). Paraclinical aspects (results of angioscanner and angio-MRI, Fisher scannographic classification). Therapeutic aspects (time to surgery, type of procedure performed: clipping and/or coating). Evolutionary aspects (post-operative deficit, cerebral ischaemia, death; functional evolution assessed by the modified Rankin score:
We began with an overall descriptive study of this series. We then identified two groups of patients whose evolutionary parameters were the subject of a comparative study: Group 1: patients who underwent intracranial aneurysm surgery between January 2013 and August 2018 and who did not undergo intraoperative microvascular Doppler monitoring of aneurysm exclusion and vascular branch patency. Group 2: patients who underwent surgery between September 2018 and December 2019 and whose surgical procedure was monitored by microvascular Doppler. II-c Statistical analysis From a prospective database of patients hospitalised for intracranial aneurysms, established since 2013, we retrospectively collected the epidemiological, clinical, therapeutic and evolutionary data of our patients. These data were recorded, analysed and formatted using Excel 2016 and SPSS IBM version 24 software. The main parameters studied related to patient outcomes, namely: post-operative deficit, ischaemia, occurrence of death and Rankin score at discharge and at one month. Bivariate analyses were performed to determine correlations using the Pearson Chi² test and the Fisher test with a significance level of 0.05. The results were then presented in the form of a table of correlations. The results were then presented in the form of tables and graphs. II-d Ethical considerations The study was previously submitted to the ethics committee of national teaching hospital Fann of Dakar for approval and confidentiality was maintained throughout the study period. Informed consent of patients and/or responsible persons was obtained for all patients. III-RESULTS III-a Epidemiological and clinical aspects: Our study included 266 patients, 83 of whom were male (31%) and 183 female (69%), corresponding to a sex ratio of 2.20. Patient age ranged from 5 to 84 years, with an average of 46 years. The 46-55 age group was the most represented, with 26.7% of patients. The paediatric population (5-17 years) accounted for 4.1% of cases (11 patients). The average hospital stay was 15.6 days, with extremes ranging from 0 to 510 days. Thirty-six percent of patients were seen within 3 days, and 29.3% were seen after 10 days. The average length of hospitalisation was 23.3 days, with extremes ranging from 2 to 113 days. Grade I was the most common in the cohort (56.2%), followed by grade III and grade II, which concerned 23% and 11.3% of patients respectively. Grade IV was less represented with only 8.3%; and no patient in our series was grade V. III-b Paraclinical aspects: Cerebral CT scan without injection of contrast medium was performed in all our patients. It revealed subarachnoid haemorrhage. This was associated with a mass effect in 10.9% of patients. With regard to Fisher’s scan classification, score 4, found in 52.6% of patients, was the most common, followed by score 3 (17.3%). (Fig.1) A total of 287 aneurysms were identified in our 266 patients by CT angiography. Aneurysms were single in 249 of our patients (93.6%) and multiple in 17 (6.4%); of these, 12 patients had 2 aneurysms and 5 had 3. The aneurysms were saccular and fusiform in 90% and 7% of cases respectively. The shape of the aneurysms was not specified in 9 cases (3.1%). Aneurysms ranged in size from 2 to 44 mm, with a mean of 7.6 mm. Medium-sized aneurysms (5-9 mm) accounted for 39.4% of all aneurysms. The preferred location was the middle cerebral artery (sylvian), which accounted for 33.1% of all aneurysms. The vast majority of aneurysms were in the anterior circulation, with 268 aneurysms (93.4%) in the anterior circulation and 19 in the posterior circulation (6.6%). (Fig.2) The average delay to surgery was 25.8 days, with extremes ranging from 1 to 510 days. Type of surgery: All patients underwent aneurysm exclusion surgery:
(Fig.3) Among the patients who underwent aneurysm surgery, 72 (27%) had their aneurysm excluded and the patency of the vascular branches checked by microvascular Doppler during the operation, while 191 (73%) did not. (Fig.4) III-d Outcomes (Analytical results) The evolutionary parameters were first studied globally for the entire cohort, then comparatively between two groups of patients. After surgery, 66 patients developed a new deficit, i.e. 24.8% of all patients. Following the operation, 34 patients (12.8%) developed ischaemia. We recorded 30 deaths during our study, giving an overall mortality rate of 11.3%. At the time of hospital discharge, 156 patients (58.6%) had a good mRS and 74 (27.8%) a poor mRS. The mRS was not specified in 6 patients and 30 of them had an mRS of 6 (11.3%). III-d-1 Short-term outcome: immediate post-op A- Post-operative deficit Among the patients who presented a new deficit in the post-operative period, 45 belonged to group 1, i.e. 23.4% of the total number of patients, and 21 belonged to group 2, i.e. 28.4% of the total number of patients; p=0.403. There was no statistically significant difference in post-operative deficit between the two groups of patients (p>0.05). B- Ischaemia Of the patients with post-operative ischaemia, 23 were in group 1 and 11 were in group 2, i.e. 12% and 14.8% of the respective numbers in the two groups (p=0.486). For post-operative ischaemia, there was also no statistically significant difference between the two groups of patients (p>0.05). C- Death Of the patients who died, 21 were in group 1, representing a death rate of 11% in this group. The remaining 9 patients belonged to group 2, bringing the death rate to 12.3% in this group. (p=0,484). With regard to mortality, there was no statistically significant difference between the two groups. Furthermore, with regard to causes of death: of the 4 patients who died of proven post-operative ischaemia, 3 were in group 1 (75%) and only one was in group 2 (25%). D- mRS at discharge At the time of discharge, the distribution of the modified Rankin score in the two groups is shown in the following table: (Table 1). So in group 1, a good mRS was defined in 111 patients, i.e. 57.8%, and a poor mRS in 56 patients, i.e. 29.1%. On the other hand, in group 2, 45 patients (60.8%) had a good mRS and 18 (24.3%) had a poor mRS, p= 0.067. The use of micro-doppler seems to improve the mRS at discharge in patients in the second group, although the difference is not statistically significant (p>0.05). Fig.5 III-d-2 Long-term evolution A- mRS at 1 month After one month’s follow-up, a good mRS was noted in 31.3% of patients in group 1, compared with 10.8% in group 2; and a poor mRS in 7.3% and 2.7% of patients in groups 1 and 2 respectively. However, the mRS at one month could not be defined in 59.3% of patients in group 1 and 79.7% in group 2; p=0.004. The use of Doppler in the second group of patients significantly improved the mRS at one month in these patients (p<0.05). IV- DISCUSSION The mean age of patients in our study was 46 years, with a peak incidence between 46 and 55 years. This observation is in line with the literature, which shows that the average age of discovery of a stroke is around 50 (i.e. young), leaving significant neurological sequelae (7; 26; 3; 23; 21). Unlike other types of stroke, subarachnoid haemorrhage is predominantly suffered by women, and the excess risk associated with women increases with age. A significantly higher incidence of SAH has been observed in women aged 55 and over (11; 24). In our study, the predominance of women was also noted, with 69% of patients being female compared with only 31% male, corresponding to a sex ratio of 2.20. The same observations were made in the Barrow study, which found a sex ratio of 2.37 (21); as well as in Ahanogbe (Togo) (3) and Waweru (Kenya) (21), who found a sex ratio of 1.33 and 1.36 respectively in their studies. The explanation for this imbalance is still unknown, but it is probably not related to the currently recognised risk factors for subarachnoid haemorrhage, namely smoking, alcohol consumption and a history of high blood pressure, all of which are more common in men than in women. Several theories suggest that this difference in incidence between the sexes may be linked to hormonal factors, although the mechanisms by which these act remain unknown (6; 14). In our series, the average hospital stay was 15.6 days, with extremes ranging from 0 to 510 days (17 months). In contrast to the series by Ahanogbe (Togo) (3), the time to admission was shorter, at 3 ± 3.69 days, as was the case in the study by Hbali (Morocco) (18), in which 78% of patients were admitted within the first 3 days. This delay in diagnosis is mainly due to a lack of knowledge of the disease on the part of many practitioners and, above all, to the unavailability of neurosurgeons and CT scanners in certain areas of Senegal, leading to erroneous diagnoses and delays in treatment. Added to this is the problem of access to care, which remains difficult for a section of the population whose average per capita income is not sufficient to cover the immediate cost of a scanner, surgery or hospitalisation. In Senegal, public health policies are much more focused on the fight against infectious diseases and maternal and child illnesses, to the detriment of neurovascular pathologies, which still suffer from a lack of investment (26). The average length of hospitalisation was 23.3 days, with extremes ranging from 2 to 113 days. In our series, one patient died after 2 days in hospital, at 3 hours post-op, of unknown cause. On the other hand, the longer or shorter hospital stay in some patients is mainly due to the complications and serious after-effects that can result from meningeal haemorrhage. In the literature, the average length of hospitalisation varies considerably. Ahanogbe (3) found that the average hospital stay was similar to ours, at 21.8 ± 20.75 days, while Waweru (Kenya) (21) found a shorter average stay of 12 days. The length of hospitalisation therefore probably depends to a large extent on the patient’s initial clinical condition and whether or not there are complications after the operation. Grade I was in the majority, found in 56.2% of patients, followed by grade III which represented 23%. Thus more than half of our patients presented with low-grade SAH in good clinical condition on admission. Only 3.8% were grade IV and no grade V patients were recorded during the study. However, this favourable initial clinical status contrasts with the delay in admission, with 29.3% of patients admitted more than 10 days after initial symptoms. Our results differ markedly from those found in the Ahanogbe (Togo) study (3), where assessment of the WFNS score revealed 45.71% of severe SAH, either grade IV or V. The Fisher score of 4 in 52.6% of patients was the most common, followed by a score of 3 in 17.3%. These results are more or less similar to those of the Sghiouar study (25) in which 42.5% of patients had Fisher grade 4 SAH. The origin of the SAH was diagnosed by cerebral angioscan. In our study, 93.4% of aneurysms were located in the anterior circulation and 6.6% in the posterior circulation, as described in the literature. In our series, 249 patients (93.6%) presented with a single aneurysm and 17 with multiple aneurysms, i.e. 6.4%; 12 of these patients had 2 aneurysms and 5 had 3. These results are comparable to those of Mudjir et al (23), i.e. 3.9%, and contrast with those of Gueye et al (15), who found a slightly higher percentage of multiple aneurysms in their series, i.e. 8.7%, and Vaz G et al (12). This low rate of multiple aneurysms in our series could be explained by the low rate of detection of small aneurysms by angioscan, which can only detect aneurysms of more than 2 to 3 mm, with a sensitivity ranging from 77 to 97% (24); the smallest aneurysms therefore go undetected. Furthermore, angiography, which can explore all the cerebral arteries and thus detect all the aneurysms present, is not available in Senegal. All our patients underwent surgery to exclude their aneurysm; of these, 74.8% underwent clipping alone, 5.6% underwent coating alone and 14.2% underwent clipping combined with coating; the average time to surgery was 25.8 days, with extremes ranging from 1 to 510 days (17 months). In the 1990s, the international ISAT study compared the results of surgical and endovascular treatment of ruptured intracranial aneurysms, revealing a lower rate of adverse clinical outcome after endovascular treatment (23.7%) than after surgical treatment (30.6%). (22) Following this study, endovascular treatment of ruptured intracranial aneurysms has gradually increased, and a recent French study showed that around 80% of ruptured intracranial aneurysms are now treated endovascularly (10). However, in our context, this issue of choice of treatment does not arise, as in Senegal, surgery remains the only therapeutic option for the management of ICA. As endovascular treatment is very recent, it is not well known and poses a real financial and medium- and long-term follow-up problem for patients who systematically choose the surgical option. The rupture of an intracranial aneurysm is one of the most frequent neurosurgical emergencies; and despite the major advances made in the understanding and management of this pathology over the last 30 years, its prognosis remains unfavourable with an overall mortality rate of around 30%; and less than 50% of patients recover all their functional abilities (2; 1). The remainder of patients suffer numerous complications, ranging from major neurological deficits to subtle cognitive and behavioural difficulties, leading to a reduced quality of life (4). In the postoperative period, the complications recorded in our patients were essentially related to the appearance of a new motor deficit, cerebral ischaemia and death. An overall analysis of these results reveals that the rate of short-term complications is higher in group 2 than in group 1; paradoxically, this is due to the fact that patients in group 2 benefited from intra-operative microvascular Doppler monitoring when their aneurysm was excluded. However, it should be noted that the sample sizes of the two groups were far from proportional, with group 1 alone accounting for almost three times the number of patients in group 2, which may partly explain these unexpected results. Thus the use of Doppler appears neither to improve functional prognosis nor to reduce mortality in these patients, contrary to what might logically be expected. Nevertheless, it is clear that microvascular Doppler seems to provide valuable intraoperative information to guide clip placement (5). At discharge, the first group had 57.8% good mRS and 29.1% poor mRS. On the other hand, in group 2, 60.8% of patients had a good mRS and 24.3% a poor mRS (p= 0.067). Analysis of these results shows that patients in group 2 had a better Rankin score at discharge than those in the first group. However, there was no statistically significant association between the use of the Doppler probe in patients in group 2 and an improvement in their mRS at discharge. At one month’s follow-up, 7.3% of patients in group 1 had an unfavourable Rankin score compared with only 2.7% with a poor mRS in group 2 (p=0.004). This time, there was a statistically significant link between the use of doppler and an improvement in the Rankin score in these patients. However, the mRS at one month could not be defined in 65% of patients, as it was not recorded in the files at the follow-up appointment. The number of missing data relating to patient progress was therefore very high. The main limitation of this study is the inequality of the samples making up the two groups, with the second group being almost three times smaller than the first. V- CONCLUSION The surgical treatment of cerebral aneurysms is currently the preferred therapeutic option for the Senegalese population because of its very affordable financial cost. This treatment is affected by complications such as the infarction of an arterial territory following an occlusion of collateral arterial branches despite a careful intraoperative exploration. The analysis of our results reveals that the use of microvascular doppler during intracranial aneurysm surgery does not reduce mortality; but has a favorable impact on improving quality of life with notably a higher score of Rankin, Both at the hospital discharge and one month post-op. 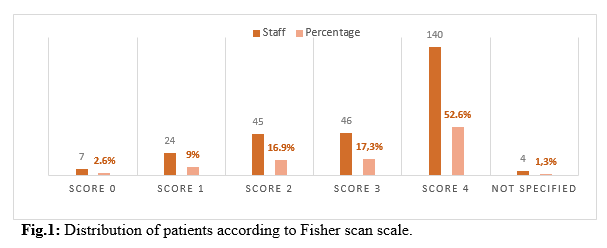 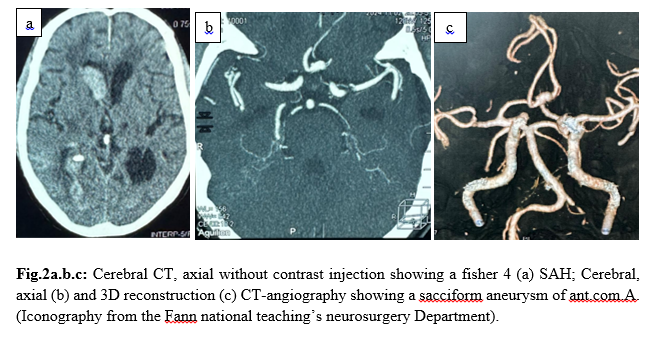 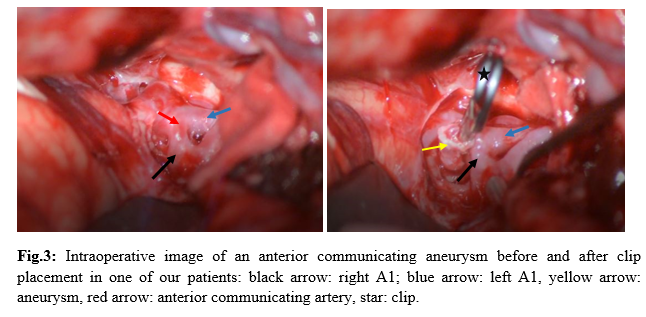 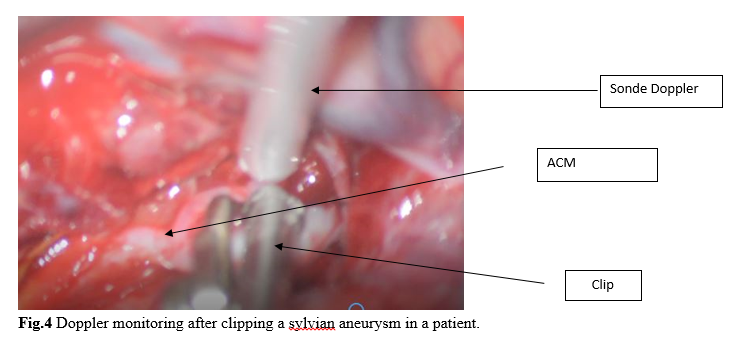 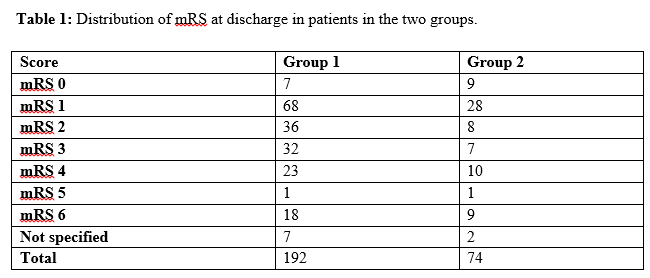 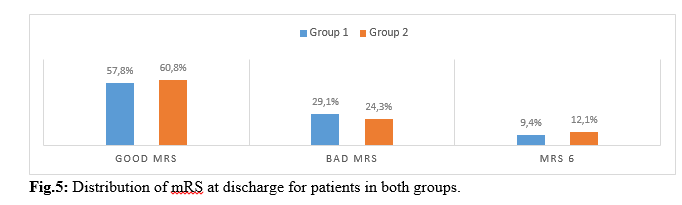 Introduction Le xanthoastrocytome pléomorphe (PXA) est une forme rare de tumeur gliale. Il représente seulement 1% des astrocytomes [4]. Selon la 5ème édition de la classification de l’organisation mondiale de la santé, le PXA est soit bénin (grade II) soit anaplasique (grade III) [14]. Cette tumeur est l’apanage de l’enfants et de l’adulte jeune et se localise dans 98% des cas au niveau de l’étage supratentoriel [19]. Les formes superficielles se développent aux dépens des leptoméninges dans 67% des cas [4]. Par conséquent, il prend un aspect à l’imagerie mimant d’autres natures lésionnelles notamment le méningiome qui constitue l’un des principaux diagnostiques différentiels. Les PXA infra tentorielles sont rares avec 29 cas répertoriés dans la littérature de 1979 en 2023 dont un seul cas pédiatrique de PXA de l’angle ponto cérébelleux (APC) [1]. Nous partageons un cas de xanthoastrocytome pléomorphe de l’APC. Apres avoir effectué des recherches dans la base de donnée de PubMed, AJOL et Google Scholar, il s’agira là, du deuxième cas de la littérature survenant chez l’enfant. Le PXA est un diagnostic à évoquer devant une tumeur de l’APC du sujet jeune. Observation Clinique : Il s’agit d’un enfant de 7 ans, qui a bénéficié d’une exérèse endoscopique de polypes nasosinusiens il y a 2 ans suite à un syndrome rhino sinusal chronique qui évoluait depuis l’enfance. Une exploration tomodensitométrie cérébrale avait permis la découverte d’une lésion de l’angle ponto cérébelleux droit qui motiva la référence du patient au service de neurochirurgie du centre hospitalier de Fann pour la poursuite de sa prise en charge. À l’interrogatoire, il présentait des céphalées chroniques d’aggravation progressive et des troubles de l’équilibre à la marche. L’examen retrouvait un syndrome cérébelleux cinétique. Cependant il n’y avait pas d’atteinte des nerfs crâniens, ni de déficit sensitif et/ou moteur. Imagerie : La tomodensitométrie (TDM) cérébrale mettait en évidence une formation tissulaire bien limitée arrondie, à base d’implantation méningée tentorielle de l’angle ponto cérébelleux droit mesurant 12x15x13 mm, hyperdense et rehaussée de manière homogène après injection de produit de contraste ( figure 1).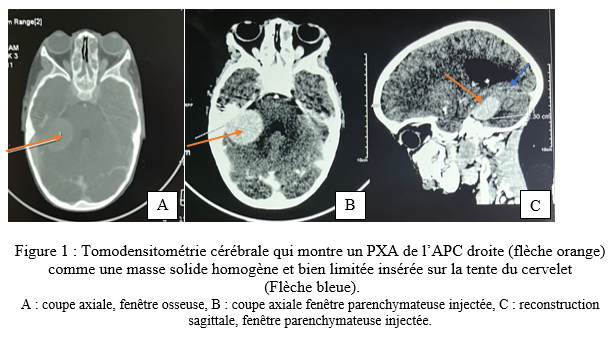 Une imagerie par résonnance magnétique (IRM) a été réalisée en complément pour mieux caractériser la lésion. L’IRM encéphalique montrait une lésion de 37,4 x 36,6 x 29,4 mm, extra axiale insérée sur la tente du cervelet à droite, iso intense en T1, hyper intense en T2 et rehaussée fortement après injection de Gadolinium (figure 2). 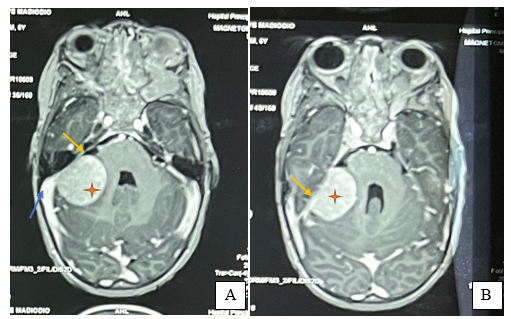 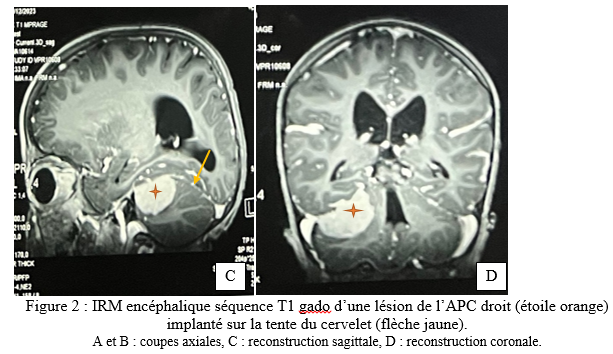 Traitement : Une craniectomie sous occipitale élargie à l’APC droit avait été réalisée. En per opératoire, nous avions identifié une lésion blanche nacrée, peu hémorragique bien limitée n’infiltrant pas le cervelet et séparée des nerfs crâniens par de l’arachnoïde. Son implantation sur la tente a été coagulée lors de l’exérèse. La tomodensitométrie post opératoire avait montré une exérèse complète et une hydrocéphalie active (figure 3). Le patient avait bénéficié d’une dérivation ventriculo-péritonéale. À Trois (3) mois de la chirurgie, l’évolution était favorable avec un amendement des céphalées et la régression des troubles de l’équilibre. À 6 mois puis à 11 mois de suivi, l’état du patient est stationnaire avec une valve fonctionnelle. 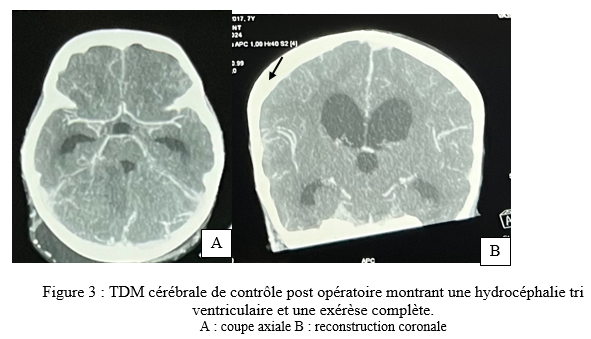 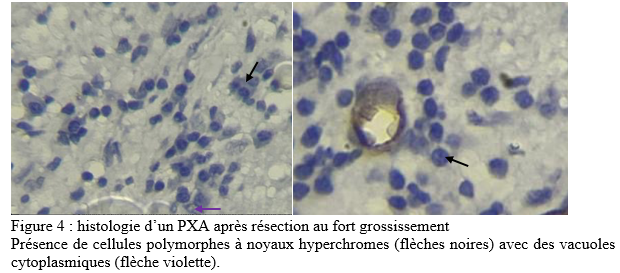 Discussion Le xanthoastrocytome pléomorphe (PXA) a été décrit pour la première fois en 1979 par Kepes et Rubinstein comme étant une tumeur astrocytaire de bas grade [7]. Il est classé parmi les gliomes astrocytaires circonscrits dans la 5ème édition de la classification de l’OMS des tumeurs du système nerveux central de 2021 [13]. Le PXA est très rare, représentant seulement 1% des tumeurs gliales et moins de 0,3% des tumeurs primitives du SNC dans le registre américain des tumeurs primitives cérébrales [17] . Il s’agit d’une tumeur de l’enfant et de l’adulte jeune avec un pic entre 10-19 ans et un âge moyen au diagnostic à 29+/-16 ans sans différence de sexe rapportée[10,19]. La présentation clinique dépend de la localisation de la tumeur et elle est commune à tout processus expansif intra crânien. Le PXA se développe majoritairement au niveau de l’étage sustentoriel particulièrement au niveau lobe temporal dans 49% des cas[4]. Chez les enfants, la fosse cérébrale postérieure notamment le cervelet est le site de prédilection du développement des tumeurs du système nerveux central. Les plus fréquentes étant d’abord le médulloblastome, l’astrocytome pylocytique, l’épendymome ainsi que l’hémangioblastome dans le cadre de la maladie de Von Hippel-Lindau. Les tumeurs de l’angle ponto cérébelleux chez l’enfant sont beaucoup plus rare. Il s’agit le plus souvent de schwanomes dans le cadre d’une neurofibromatose, de kystes dermoides ou épidermoides, de tumeurs rhabdoides tératoides et des gangliogliomes [8]. A cette liste, nous pouvons ajouter les PXA. Dans une revue de 1979 à 2023, 29 cas de PXA de la fosse cérébrale postérieure ont été répertoriés[1]. La tumeur de notre patient était localisée au niveau de l’APC alors que deux cas seulement étaient retrouvé dans la littérature dont un cas pédiatrique décrit par Kurschel en 2006 [11]. La majorité des PXA de l’angle ponto cérébelleux étant associée à un gangliogliome et sont appelés des formes composites [5]. L’aspect commun du PXA à l’imagerie est un kyste avec un nodule mural prenant le contraste[14]. Cependant, l’imagerie des PXA de la fosse cérébrale postérieure n’ont pas beaucoup été détaillés dans la littérature car cette localisation reste encore exceptionnelle. Les rares cas décrits ont des localisations surtout médianes ou hémisphériques dans le cervelet. Il se présente habituellement comme une masse charnue isodense à la TDM et en signal intermédiaire à l’IRM rehaussée après injection de contraste [6,10]. La lésion présente une double composante kystique et charnue chez le cas publié par kurschel [11] alors qu’elle était purement solide chez notre patient. Il n’y a pas de caractéristiques spécifiques décrites concernant le rehaussement leptoméningé des PXA. Par rapport aux méningiomes qui représentent leur principal diagnostic différentiel, le signe de la queue durale est présente dans 67% de PXA avec une atteinte des trois feuillets méningés dans 13% des cas [18], ce qui rend difficile leur diagnostic. Le PXA serait issu des astrocytes sous piales expliquant son développement superficiel et impliquant à des degrés variables les leptoméninges. La tumeur infiltre le parenchyme et s’étend dans les espaces péri vasculaires [4]. Son pléomorphisme est lié à la présence de cellules fusiformes et de cellules géantes multi nucléés, contenant des vacuoles lipidiques avec des dépôts de corps granuleux éosinophiles et réticuliniques. À l’immunohistochimie la positivité des marqueurs GFAP ( protéine de l’acide fibrillaire gliale) et PS100 indique l’origine astrocytaire de la tumeur [7]. De plus, il existe des altérations génétiques comme la mutation BRAF V600E et la délétion homozygote de CDKN2A et/ou CDKN2B impliquées dans l’activation de la voie de signalisation MAPK. Et, la forte prévalence de ces mutations explique leur association fréquente à la neurofibromatose de type 1[20]. Chez notre patient, la recherche d’une mutation BRAF et d’une neurofibromatose nous aurait permis de vérifier cette thèse. Près de 77% PXA sont bénins (grade II histologique) définis par un index mitotique <1% selon la classification OMS 2021. La forme anaplasique ou grade III implique la présence de nécrose et/ou de plus de 5 mitoses pour 10 champs [16]. A ce jour, il n’existe aucune technique codifiée de résection des PXA. L’idéal est une exérèse macroscopiquement totale. Il constitue un des facteurs pronostiques majeurs de survie sans récidive. Chez notre patient une résection complète par morcellement suivie de la coagulation de l’insertion méningée a été réalisée. En effet, même si le PXA est généralement de bon pronostic, plusieurs revues ont confirmé le grade histologique, l’âge et l’étendue de la résection comme étant les facteurs pronostiques significatifs sur la survie globale et la survie sans récidive des malades [3]. Dans une méta-analyse portant sur 325 patients, la survie sans progression et la survie globale à 5 ans est de 51,2% et 78% respectivement. Les patients de moins de 20 ans et ceux qui ont bénéficiés d’une résection macroscopiquement totale ont une meilleure survie[16]. Ainsi, le taux de récidive sur les PXA grade II partiellement réséqué est plus élevé comme démontré dans l’étude de Lee et al [12]. Les PXA grades III anaplasiques représentent 10 à 20% des PXA et peuvent survenir de novo ou par transformation des grades II dans 20% des cas [6]. Leur pronostic est moins favorable avec une survie médiane à 49 mois contre 209 mois pour les grade II [15]. Les formes évolutives et récidivantes sont pourvoyeuses de métastases léptoméningées, d’où l’intérêt d’une IRM encéphalo medullaire dans le bilan d’extension avant une radio chimiothérapie adjuvante. De nombreuses études rejettent le recours systématique de la radiothérapie et/ou chimiothérapie adjuvante dans les PXA grade II. Elles n’ont aucun impact significatif dans l’amélioration de la survie des malades[1,3–8]. Au contraire, elles peuvent être délétères chez les sujets âgés et réduire leur survie [9]. Cependant, la radiothérapie cranio-spinale en cas de dissémination leptoméningée et la chimiothérapie dans les formes évolutives restent indiquée chez le sujet jeune. Chez notre patient, un traitement adjuvant n’était indiqué après avis de la réunion de concertation multidisciplinaire en oncologie pédiatrique. Toutefois, une surveillance est de préconisée afin de détecter précocement une récidive sur le long terme. Cependant, l’utilisation des inhibiteurs BRAF comme le vemurafinib ou dabrafenib, est associée à un meilleur pronostic des PXA avec mutation BRAFV600E [2]. Toutefois d’autres études sont nécessaires afin de trouver une relation entre l’utilisation de cette thérapie ciblée et la survie globale des patients. Conclusion Le xanthoastrocytome pléomorphe de l’angle ponto cérébelleux chez l’enfant est exceptionnel. Ses caractéristiques radiologiques peuvent facilement prêter à confusion avec des types de tumeurs beaucoup plus fréquents notamment le méningiome ou le schwannome vestibulaire. Ce cas démontre l’intérêt d’évoquer le PXA devant toute tumeur de l’APC car son pronostic dépend essentiellement de l’approche chirurgicale en dehors du type histologique. Une exérèse macroscopiquement totale garantit une survie meilleure. Articles récents
Commentaires récents
Archives
CatégoriesMéta |
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647