NEUROLOGICAL MANIFESTATIONS HIV-INFECTED PATIENTS AROUND VARANASI, INDIAABSTRACT
Background
Most of the studies on the neurological manifestations in HIV patients in India were cross sectional in design, and focus on the etiological agents. We report data on the frequency of neurological manifestations, associations with CD4 counts, and outcome of its various presentations in a 3-year prospective hospital-based study.
Methods
All HIV-infected patients attending the Infectious Disease clinic for various neurological manifestations between Jan 2001 and December 2003 were included in the study. Their clinical details, treatment received, and response to treatment were accessed and analyzed.
Results
During this period, 57 had some neurological manifestations and made 145 clinic visits, with 158 distinct episodes of neurological related symptoms, giving a crude rate of 307 neurological episodes per 1000 person year of observation
Conclusion
Opportunistic infections were the leading cause of neurological disorders in our study population. Apart from Central nervous system (CNS) tuberculosis, other CNS diseases were good predictor of the advanced HIV infection (CD4<200). CNS tuberculosis cannot be considered as an opportunistic infection in most of the instances as it can be seen in relatively earlier stages of the disease. Cerebrospinal fluid picture was normal in all our patients of CNS toxoplasmosis. All the patients with progressive multifocal leuco encephalopathy had seizures as the initial manifestation. AIDS-dementia complex and CNS malignancies were not observed in our patients. There were equal responses to Amphoterecin B Cholesterol Dispersion (ABCD) and conventional Amphoterecin B therapies, and no significant differences in their side effect profiles.
Key words: infections, HIV, India
Key words: infections, VIH, Inde
INTRODUCTION
India is estimated to have more than 60,000 full-blown AIDS cases by the end of 2005, and this makes it one of its fast growing health problems (13) NACO 2005). The clinical spectrum of HIV infection in India is different from rest of the world, and regional variability has been reported within India (1,2,6,10,11,14,15,16) Central nervous system (CNS) infections are the third commonest cause of morbidity and second commonest cause of mortality in HIV patients (13). There has been no prospective study so far to determine the frequency and pattern of CNS infections in HIV patients in eastern Uttar Pradesh and western Bihar regions. This study was therefore undertaken to provide such baseline information.
METHODS
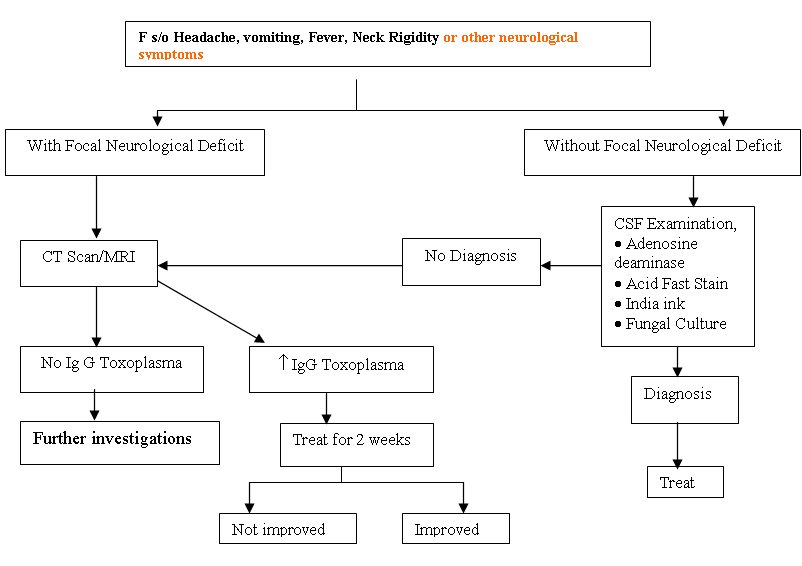
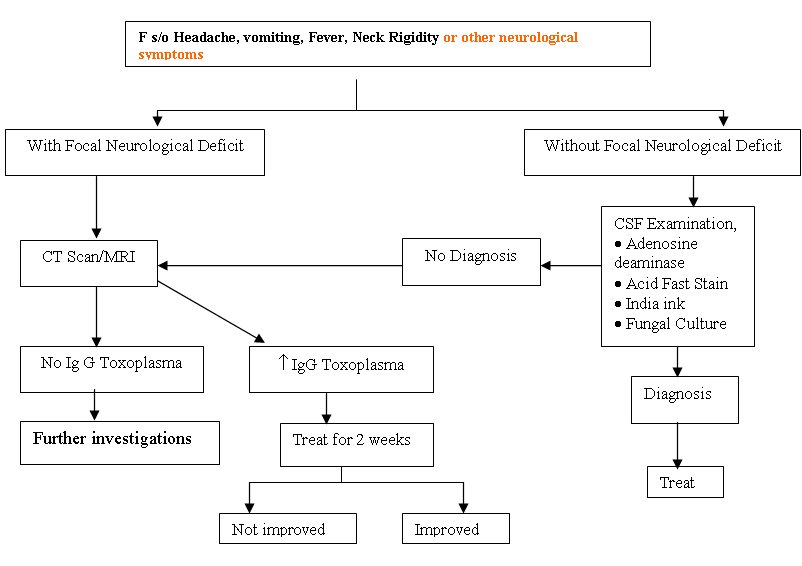
All HIV infected patients attending the Infectious Disease clinic for various neurological manifestations were included in the study. Sir Sunderlal hospital, affiliated to Institute of Medical Sciences, Banaras Hindu University is a tertiary care teaching hospital with catchments area of five states (Uttar Pradesh, Madhya Pradesh, Bihar, Jharkhand, and Chattisgarh) with 1000 beds. The annual attendance of new HIV cases is approximately 150. HIV related CNS diseases, clinical characters and the treatment outcomes were registered. An informed consent was taken from all the subjects of study prior to investigative procedures. The general work up protocol followed in this study was outlined as below.
Diagniostic criteria followed
Diagnosis of tubercular meningitis was based on history of sub acute or chronic meningitis, cerebrospinal fluid (CSF) showing increased protein levels, lymphocytic pleocytosis along with raised Adenosine deaminase levels above 7 IU/L, and presence of acid fast tubercular bacilli (AFB). Cryptococcal meningitis was diagnosed by India ink method, or culture demonstrating Cryptococcus or both. Toxoplasmosis was diagnosed by CT/MRI showing multiple ring enhancing lesions, raised Ig G levels and response to treatment. Progressive multifocal leukoencephalopathy was diagnosed by MRI. However we did not perform neuropathological studies of biopsied brain tissue owing to cultural and ethical constraints. Individuals who had no specific identifiable diagnosis were classified as Undiagnosed
CD4 / Viral load estimation
Immuno phenotype of lymphocytes was carried out by FACS count (Becton Dickinson, Singapore (BD). Viral load was not done due to economic constraints.
RESULTS
The study population of 375 patients consisted of individual who had come forward, with the HIV related symptoms. There were no differences in age sex, or clinical stage between patients with and without neurological deficits therefore further comparison was not made. All the patients in the present study were on HAART as all of them have AIDS. During this period, 57 had some neurological manifestations and made 145 clinic visits, with 158 distinct episodes (defined as any visit for the symptoms, for which the etiology or the outcome could be attributable to nervous system), giving a crude rate of 307 neurological episodes per 1000 Person years of observation. The clinical profile of the patients is shown in Table 1.
Table 1: Neurological manifestations
| Symptoms/sign (number of patients) |
CCM (n=16) |
TBM (n=25) |
Toxoplasma (n=5) |
PML (n=3) |
Undiagnosed (n=8) |
| Fever (42) |
12 (75%) |
23 (92%) |
1 (20%) |
0(0%) |
6 (75%) |
| Headache (40) |
14 (87.5%) |
20 (80%) |
2 (40%) |
0(0%) |
4(50%) |
| Focal Neurological Deficit (13)[barring cerebellar signs] |
2 (12.5%) |
6 (24%) |
5 (100%) |
0(0%) |
0(0%) |
| Cerebellar signs (5) |
1 (6.25%) |
1 (4%) |
0 (0%) |
3 (100%) |
0(0%) |
| Increase Intracranial Tension with meningeal signs (40) |
14 (87.5%) |
21 (84%) |
1 (20%) |
0 (0%) |
4 (50%) |
| Seizure (26) |
8 (50%) |
7 (28%) |
2 (40%) |
3 (100%) |
6 (75%) |
| Altered sensorium (18) |
6 (37.5%) |
9 (36%) |
3 (60%) |
0(0%) |
0(0%) |
| Papilloedema (20) |
8 (50%) |
10 (40%) |
0 (0%) |
0(0%) |
2 (25%) |
CCM = Cryptococcal Meningitis
TBM = Tubercular Meningitis
PML = Progressive Multifocal Leucoencephalopathy
All the patients of PML had seizures and cerebellar symptoms only at presentation there by making PML as one of the important differential diagnosis in all patients with those symptoms in our population. In a similar way presence of fever indicates either CCM or TBM, as most of our patients have either of them. Headache is fairly common in all the patients barring those having PML. Presence of focal neurological deficits (probably secondary to the toxoplasm bodies) strongly argue in favor of toxoplasmosis, the second commonest diagnosis being TBM.
Cerebrospinal fluid examination results were expressed in the below table
Table 2: Cerebrospinal fluid (CSF) findings
| CSF finding |
CCM (n=16) |
TBM (n=25) |
Toxoplasma (n=5) |
PML (n=3) |
Undiagnosed (n=8) |
| Cells (/mm3) |
20±6 |
97.4±49.4 |
6.8±1.3 |
6.8±1.3 |
8±2 |
| Neutrophils (%) |
0 |
4±6 |
0 |
0 |
0 |
| Lymphocytes (%) |
100 |
95±6 |
100 |
100 |
100 |
| Protein (mg/dl) |
68.6±26.2 |
186±67 |
81±14 |
81±14 |
42±2 |
| Sugar (mg/dl) |
10.3±7.2 |
30±8 |
29±8.9 |
29±8.9 |
68±24 |
| India ink |
+ve in 15/16 |
– ve |
-ve |
-ve |
-ve |
| ADA (IU/L) |
3 |
8 |
2 |
3 |
0 |
| CD4 (Mean ± SD) |
135± 64 |
190 ± 170 |
115 ± 82 |
104 ± 61 |
– |
| CD4 Range |
12-245 |
30-610 |
12-241 |
35-153 |
– |
All the patients with tubercular meningitis had marked lymphocytic pleocytosis (mean cell count of 97.4±49.4) along with raised protein levels (mean 186+67). ADA levels were raised markedly in all the cases (8). In CCM although pleocytosis was seen, it was not so high as in cases of tuberculosis (20+6). There was a mild elevation in protein content, but CSF sugar levels were extremely low (10.3+7.2. CNS toxoplasmosis was suspected in 5 patients with focal neurological deficits. In all the patients, MRI/Double contrast CT showed multiple ring enhancing lesions and IgG levels for Toxoplasma was markedly raised. Four patients responded to therapy. All the patients of progressive multifocal leuco encephalopathy had cerebellar signs, and seizures. Diagnosis was made by MRI. In 8 patients the etiology could not be made out as the patients expired on the very same day of admission and were labled as undiagnosed.
The positive predictive value of the various neurological disorders in predicting the CD4 levels of less than 200 were represented in the table 3 and was compared with other AIDS defining illnesses.
Table 3: Specificity and positive predictive value of few neurological conditions
| Disease |
Specificity (%) |
Positive predictive value (%) |
| PML |
100 |
100 |
| Cryptococcal Meningitis |
98.1 |
81.25 |
| CNS Toxoplasmosis |
99.3 |
80 |
| Tubercular meningitis |
93.86 |
73.4 |
| Candidiasis |
69.3 |
38.27 |
| Recurrent Herpes Zoster |
97.5 |
66.6 |
| Molluscum Contagiosum |
99.3 |
83.3 |
| Tubercular Lymphadenitis |
87.1 |
8.6 |
| PCP |
97.5 |
71.4 |
Table 4: Treatment outcome in different neurological conditions
| Disease |
Treatment |
No. of patients |
Response: Improved |
Response: Not improved |
Response: Lost in follow up |
Response: Expired |
| CCM |
Ampho B |
6 |
4 |
0 |
0 |
2 |
| |
ABCD |
6 |
4 |
0 |
1 |
1 |
| |
fluconazole alone |
4 |
0 |
0 |
4 |
0 |
| TBM |
RHEZ+Q+S |
18 |
9 |
2 |
5 |
2 |
| |
RHEZ+S |
7 |
3 |
2 |
1 |
1 |
| Toxoplasma |
Pyremethamine +Clindamycin |
5 |
4 |
1 |
0 |
0 |
| PML |
HAART |
3 |
1 |
0 |
2 |
0 |
ABCD= Amphotericin B Cholesterol Dispersion
RHEZ = Rifampicin +Isoniazide +Ethambutol +Pyrazinamide
S=Streptomycin
Q= Quinalone (ciprofloxacin)
HAART = Highly active antiretroviral Therapy
Most of the patients with TBM in the present study who had a high GCS at presentation improved better with treatment (10/15) when compared with those who came with low GCS (2/10). Out of the 16 patients who presented with the CCM, 4 patients refused any treatment so they were prescribed oral fluconazole desperately. 12 patients were offered Amphoterecin B (6 patients received ABCD + 6 patients received conventional Amphoterecin B). 4 patients from each group survived (total of 8 patients). Out of them 3 patients are still in follow up for more than 13 months. The remaining 5 patients were lost to follow up. Out of the 4 patients who did not respond, 3 patients expired during the treatment and 1 patient left against medical advice. All the patients of PML were prescribed HAART. Single patient is on follow up after 1 year, but 2 patients were lost to follow up after a median period of 5 months. Only a single patient of toxoplasmosis did not responded favorably to the therapy rest all showed complete response to therapy.
DISCUSSION
HIV infection of the CNS results in damage to the nervous tissue and there has been a geometrical increase in the incidence and recognition of neurological disorders in HIV infected individuals over the past decade (14). Majority of the present study population were in advanced stage of HIV disease (AIDS), confirmed by clinical staging and CD4 level. In India the HIV prevalence in males is higher than females (13) so as in the present study where the male female ratio was 3.7:1. Therefore, females and early HIV infection were under represented in the present study. The CNS involvement is broadly classified into three groups viz by HIV, by opportunistic infections and by malignancies.
Opportunistic infections:
With the advent of HAART the incidence of opportunistic infections decreased remarkably in west with non infectious etiologies leading the list of neurological manifestations. However in countries like India where the prevalence of opportunistic infections is high, it is not surprising to see them leading the list of etiology of neurological conditions (1,2,6,10,11,14,15,16) as observed in our study (46/57 i.e. 81%).
CNS Tuberculosis
CNS tuberculosis can be seen at all stages of the disease (5). Associated intracranial mass lesions suggestive of tuberculoma are more commonly reported in HIV positive individuals (60% vs 14%) as compared to those with seronegative TBM (14) But in the present study only single patient (4%) had tuberculoma which is far less compared to the literature. We found that ADA is a better marker to predict response as the mean levels in patients who responded to anti tubercular therapy (ATT) were 9 IU/L compared with those who did not respond (mean level was 6 IU/L). The level of sensorium was also an important marker of outcome. Most of the patients in the present study who had a high GCS at presentation improved better with treatment (10/15) when compared with those who came with low GCS (2/10).
CCM
The incidence of cryptococcal meningitis varies from 5-28% in different countries (14, 11, 15, 1, 10, 16, 6) In the present study seizures were found more frequently than other studies. Amphoterecin B is the main stay of the treatment in CCM. The introduction of liposome form of Amphoterecin has shown promising results without some of the serious adverse effects (4) though the clinical data are insufficient. We observed similar responses with ABCD and the conventional Amphoterecin B, and interestingly no differences in the side effect profile. In view of the small sample size, further speculation is not made here.
CNS toxoplasmosis
The incidence of toxoplasmosis in different studies has been from 1.33% to 3.3% (15, 11, 15, 1, 10, 16, 6) The incidence in the present study was 1.33%, comparable to rest of Indian studies. One of the interesting features is that CSF picture was normal in all our patients.
PML
PML is one of the rare CNS related disorders observed commonly in HIV patients, caused by JC virus. The favorable prognosis in PML include a CD4+ count >100/ L at baseline and the ability to maintain a HIV viral load of <500 copies per milliliter (7). Similar was our findings and only a single patient out of 3 with PML is doing well as his CD4 levels are 182. All the patients of PML in the present study had seizures as their first manifestation, though it is not a gray matter disease. The possible reasons for seizures could be the demyelinated lesions adjacent to the cerebral cortex acting as irrigative foci, axonal conduction abnormalities, or disturbance of the neuron-glia balance. Moulignier et al also reported 10 HIV patients with PML, presenting with partial or generalized seizures as the first neurological manifestations (12)
Immune Status and CNS diseases:
Opportunistic infections of the CNS, probably with the exception of cryptococcal meningitis usually follow reactivation of latent infections (14). This suggests that a defect in immunoregulation is the principal mechanism leading to the development of opportunistic infections. This was also supported by the finding of the present study that most of the CNS infections (45/57 i.e.79%) occurred at CD4 levels of less than 200. However, a small number of patients (11/57) with a CD4 count between 200 and 500 also had CNS infections (most of them were tubercular meningitis (7 cases), cryptococcal meningitis (3 cases) and a single case of toxoplasmosis). Moreover, the CD4 count in all the patients with cryptococcal meningitis and toxoplasmosis was in the range of 200-250, suggesting a severe immunocompromized state. However CNS tuberculosis cannot be considered as an opportunistic infection in most of the instances as it can be seen in relatively earlier stages of the disease. Barring CNS tuberculosis, any other CNS disease is reasonably good predictor of the advanced HIV infection (CD4<200). Similar observations were made by various other authors across the globe and the inclusion of tuberculosis in clinical case definition of AIDS in countries where the disease is endemic was questioned in prospective and retrospective studies (3).
HIV induced CNS diseases
Primary processes related to HIV infection of the nervous system are reminiscent of those seen with other lenti viruses, such as the Visna- Maedi virus of sheep (9). HIV can affect practically every part of the nervous system ranging from cognitive dysfunction AIDS dementia complex (CNS) to the autonomic neuropathy. It is important to point out that evidence of infection of the CNS with HIV does not imply its role in causation of the disease as 90% of the HIV patients have CNS involvement by HIV though most of them are asymptomatic (9).
The AIDS dementia complex, reported in 66% of the western population is uncommon in India (13%). The rapid improvement in cognitive function noted with the initiation of antiretroviral therapy suggests that at least some component of this problem is quickly reversible (9).We did not encounter even a single case of AIDS dementia complex in our cohort of patients, though majority of our patients were in relatively advanced HIV infection. We could not explain this seemingly paradoxical finding and still studying the cause for the same.
HIV related CNS malignancies
The exact incidence of the CNS malignancies in HIV patients from various parts of India is largely unknown but defiantly les than the west. The non uniform performance of the neuropathological studies, lack of facilities for the diagnosis in most of the centers might contribute to this to some extent. But in the present study also we couldn’t find even a single case of HIV related CNS malignant condition.
CONCLUSION
1. Opportunistic infections are still the leading cause of neurological disorders in our population
2. CNS tuberculosis cannot be considered as an opportunistic infection in most of the instances as it can be seen in relatively earlier stages of the disease. Barring CNS tuberculosis, any other CNS disease is reasonably good predictor of the advanced HIV infection (CD4<200).
3. CSF picture was normal in all our patients of CNS toxoplasmosis.
_4. All the patients with PML had seizures as the initial manifestation
5. AIDS dementia complex and CNS malignancies were not observed in our population
6 We observed similar responses with ABCD and the conventional Amphoterecin B, and interestingly no differences in the side effect profile
SOME CLINICAL AND PSYCHOSOCIAL DETERMINANTS OF INDEPENDENT WALKING ATTAINMENT BY POST STROKE PATIENTSABSTRACT
Background
It is not uncommon for post stroke patients or their caregivers to ask the attending physiotherapist when the patient would regain ability to walk. This is often difficult to predict as many clinical and non-clinical factors influence when this function is accomplished.
Objective
To investigate the influence of some clinical and psychosocial factors on the time post stroke individuals commence independent walking.
Methods
The one-group, pre-experimental study carried out in a teaching hospital facility involved 27 (14 males and 13 females) fully conscious, unilateral, first-episode stroke patients admitted to the facility and referred for physiotherapy over 5 months. A daily, structured physiotherapy care including Bobath technique was administered on the patients for 12 weeks. Ages, marital status, years of formal education, occupation, personality type (Eysenck classification), level of disability, co-morbid factors and admission-referral interval were obtained. Main outcome measure was time taken to attain ability to walk a continuous, level floor 10m distance unaided.
Results
The mean time independent walking was attained was 7.4 ± 2.6 weeks. Participants with mild disability level at baseline commenced independent walking significantly earlier (4.00 ± 0.01 weeks) than those with moderate disability (7.72 ± 2.53 weeks). Independent walking attainment time showed no significant difference (p>0.05) across the psychosocial factors. A significant relationship were found between age (r = – 0.57), functional independence measure (r = – 0.55) and commencement of independent walking.
Conclusion
Age and the initial level of disability had significant influence on commencement of independent walking by the participants.
Key Words: Africa, Independent Walking, Psychosocial, Stroke
RESUME
Introduction
Il n’est pas inhabituel pour les patients victimes d’un accident vasculaire cérébral (AVC) et pour leur soignants, de demander aux rééducateurs fonctionnels le délais permettant la reprise de la marche. Ce délai est souvent difficile à prévoir compte tenu des facteurs multiples, à la fois cliniques et non cliniques intervenant dans cette fonction motrice.
Objectif
L’objectif est de définir quelques facteurs cliniques et psychologiques influençant la durée de récupération post-AVC permettant l’autonomie de la marche.
Méthodes
Un groupe préliminaire a été étudié dans un centre hospitalier universitaire et concernaient 27 patients (17 mâles et 13 de sexe féminin) conscients, présentant un déficit unilatéral après un premier épisode d’accident vasculaire. Il ont été suivis dans un centre de physiothérapie durant cinq mois. Une prise en charge quotidienne incluant la technique de Bobath a été instituée pendant douze semaines. Les paramètres suivants ont été étudiés : âge, statut marital, niveau de formation et d’éducation, profession, personnalité (classification d’Eysenck), degré d’invalidité, facteurs de co-morbidité, et de délai de prise en charge.
La principale mesure attestant de la capacité à marcher de manière continue a été une marche continue, sur distance plane de 10 mètres, sans aide.
Résultats
Le temps moyen de reprise de la marche sans aide était de 7.4 ± 2.6 semaines. Les patients avec un handicap moyen ont eu une récupération plus précoce modéré (4.00 ±0.01 semaines) que ceux qui avaient un handicap (7.72 ± 2.53 semaines). Les facteurs psychosociaux n’étaient pas significatifs (p>0.05). Une relation a été objectivée entre l’âge (r = – 0.57), le degré d’indépendance (r = – 0.55), et le début de la marche de manière autonome.
Conclusion
L’âge et le degré d’invalidité avaient une influence significative sur le délai de reprise d’une marche autonome.
Mots clé : Accident vasculaire cérébral, Afrique, Autonomie, facteurs psychosociaux, Marche, Nigéria, Réeducation fonctionnelle.
INTRODUCTION
Stroke is an important cause of long-term disability worldwide, as it results in considerable impairment of sensory, motor, mental, perceptual and language functions [11]. Loss of mobility, major motor function impairment in this group of patients, is closely related to specific medical and non-medical factors such as age 75 years and above, and existence of cognitive disorders [9]. Interventions to improve motor function and mobility therefore forms an important component of stroke management and rehabilitation lead to improved movement pattern regardless of sex, co-morbidity and initial severity of stroke [10].
Independent walking is often used as an indicator of functional recovery in stroke. It is not uncommon for the stroke patients or their carers to ask the Physiotherapist managing the patient when s/he would regain ability to walk. The time this level of function will be attained is usually difficult to predict as many clinical and non-clinical factors such as socio-demographic attributes [2] exert significant influence on stroke outcome, including when the patient would commence independent walking. For example, a study by Warlow [13] had concluded that age; initial mild deficit and early resolution of symptoms, as well as absence of cognitive impairment are good prognostic signs at two weeks post stroke. A retrospective study had also observed that the neurological outcome of stroke was poorer in patients who have diabetes mellitus as co-morbidity than those without [4]. Psychological problems such as mood disorders are reported to have negative impact on rehabilitation outcome [12], while socio-cultural issues like gender-based traditional roles and responsibility assignment practice, as may be found in some cultures including Africans, have also been identified to have potentially significant influence on a post stroke individual in terms of motivation to become independent.
Whereas various studies have been carried out on mobility after stroke, there is paucity of an individual study that considered how some clinical and psychological factors influence the time taken to recover independent walking by individuals who have suffered a stroke. This study was aimed at investigating the possible influence of selected psychosocial and clinical factors on commencement of independent walking in individuals who have suffered a stroke. Specifically this study considered the possible influence of age, marital status, educational qualification, occupation, personality type, disability status, and co-morbidity on recovery of this functional ability. Independent walking was defined in this study as ability to walk a distance of 10 metres on a level floor continuously and unaided.
MATERIALS AND METHODS
Participants
Twenty-seven (14 males and 13 females), unilateral and first episode, freely consenting in-patient stroke victims referred for physiotherapy at the University College Hospital Ibadan, Nigeria were consecutively recruited over a period of 5 months. Ten of them had left-sided and 17 right-sided hemiplegia; 19 had suffered ischaemic while 8 had haemorrhagic CVD, radiologically or clinically diagnosed by the neurologist in charge of the patients.
Only subjects who met the underlisted inclusion criteria participated in the study:
a. Individuals with hemiplegia resulting from first incidence of stroke.
b. Subjects who were not independently ambulant at the time of referral but fully conscious and well oriented in time and place, and had no difficulty communicating and comprehending instructions.
Procedure
The protocol of this study was approved by the Joint Ethical Committee of the University of Ibadan/University College Hospital, Ibadan, Nigeria (IRC Protocol No: UI/IRC/03/0080). Every new stroke patients referred for physiotherapy was initially evaluated by one of the authors to determine whether they meet the study criteria or not. The procedure involved was explained to the prospective participants who satisfied the inclusion criteria before obtaining their informed consent. They were however blinded to the main outcome measure (independent walking attainment time). The following parameters were obtained at the point of recruitment:
Social Factors: Age in years, sex, marital status, level of formal education, total years of education and occupation. Occupations were categorized into: Trading; civil-service; artisan; retired.
Psychological Factors: The personality type of the patients was determined using the Eysenck personality type questionnaire (EPQ). A validity of 0.9 and internal consistency of 0.84 has been reported for this instrument [3]. It was researcher-administered and each subject responded to the questions by answering either “Yes” or “No”. A score of 1 was given to “Yes” and zero to “No”. The total score was added up in each category of 4 different personality types- introvert, extrovert, psychotic and neurotic. The personality type where the subject scored the highest determined his/her personality.
Clinical Factors: Side of affectation, presence of co-morbid factors (hypertension and or diabetes mellitus only), the time interval between admission to the hospital and when referred for physiotherapy (admission-referral interval) were also determined, as appropriate, from physical examination and the medical records of each participant.
Level of disability was determined by administering the functional independent measure (FIM) instrument, which assesses the physical and cognitive level of disability in the hemiplegic stroke subject. Each subject was asked to perform the basic life activities listed on the FIM instrument and scored accordingly. The FIM has a reliability coefficient of 0.93 and a validity score 0.84.
Structured Physiotherapy Intervention
Each participant received structured physiotherapy care. This included positioning in bed, respiratory physiotherapy and functional mobility activities which were based on the Bobath approach to management of hemiplegia. Treatment was administered daily, each session lasting 45 minutes. This was continued until the subject was ready to commence walking. Independent walking was determined by asking the subject to perform a continuous 10-metre floor walk in the physiotherapy gymnasium at his/her self selected walking velocity and without any assistive device or support from the therapist. The duration of participation in this study by each subject was 12 weeks. This is the most common upper limit admission time for stroke patients receiving physiotherapy at this hospital facility. Treatment of individual patient however continued until discharge from the physiotherapy unit on out-patient basis.
Obtained data were analysed using SPSS package. Mann-Whitney U, Kruskal-Wallis and Pearson correlation coefficient (r) were calculated, as appropriate, at 0.05 alpha.
RESULTS
Twenty eight participants were recruited but one of them could not complete this study, as he was transferred to another hospital upon request by his family members. The results presented in this report are therefore with respect to the 27 subjects (13 females and 14 males) that completed the study.
The mean quantifiable parameters of the participants such as age, independent walking attainment time and admission-referral interval are presented in table 1. The results of Mann-Whitney U statistical test as presented in table 2 shows that participants with mild disability level at baseline commenced independent walking earlier than those with moderate disability (p<0.05). Comparison of independent walking attainment time by psychosocial factors showed no significant difference (p>0.05) across these factors (Table 3). Correlation analysis using Pearson product moment correlation coefficient (r) showed that both age and functional independence measure have statistically significant association (p<0.05) with independent walking attainment time (Table 4).
DISCUSSION
One of the indicators of functional recovery from stroke is independent walking, which promotes discharge home. Many clinical and non-clinical factors would affect when this functional level is attained. The objective of this study was to investigate the influence of some clinical and psychosocial factors on the time independent walking was attained by stroke patients who received a 12- week structured physiotherapy care. In this study, independent walking was taken to be ability of a stroke patient to walk a distance of 10 metres unaided and continuously.
The mean time for commencement of independent walking was 7.4 ± 2.6 weeks in this study. Whereas no statistically significant sex differential was observed in the time of commencement of independent walking, it took the female participants a longer period (7.92 ± 2.81 weeks) than their male counterparts (7.00 ± 2.54 weeks) to achieve this task. Only 25% of the participants commenced walking within five (5) weeks and 70% within twelve (12) weeks of the structured physiotherapy care. Pomeroy and Tallis [10] had reported that 56% of their stroke patients regained independent walking 6 weeks after referral to physiotherapy. In general the time independent walking status is attained by stroke victims differ greatly and this variation can be attributed to several factors such as age, severity of the stroke, co-morbidity and rehabilitation approach. Differences in these factors may account for the disparity in the result of this study and the earlier report [10].
Age was found to have a negative correlation with time of commencement of independent walking, suggesting that the older the subjects, the earlier they commence independent walking. Contrary to this observed trend, a previous report had concluded that the cumulative effects of aging on the cardiovascular system and many chronic illnesses commonly seen in older adults are predictive of worse functional outcome, longer length of stay in the hospital and greater disability following rehabilitation [8]. The disparity in the findings may be attributed to other associated psychosocial and clinical factors that vary in the stroke subjects in these two studies.
Each of marital status, level of formal education, total years of education and occupation had no significant influence on time of commencement of independent walking, and by inference are not determinants of this important measure of functional recovery. Other studies had however reported that socio-economic factors [6] and the presence of a spouse at home [5] are factors that may accelerate functional recovery and discharge home of stroke patients. In this study only one-fifth of the patients were not married. This non-significant difference in the marital status of the patients could have accounted for the non-difference observed in the recovery time of independent walking across marital status. In addition, unlike the earlier study[5] which identified presence of a spouse at home as a positive influencing factor on recovery from stroke, the participants in this present study were still hospitalized at the time of this study. Therefore, the likely influencing effect of a spouse at home on recovery may not be established at this stage of recovery. The distribution of participants by occupation and level of formal education was also not significantly different in this study.
The side of affectation, admission-referral interval and co-morbid factors did not significantly influence the time of commencement of independent walking by our subjects. However we observed that the subjects who had hypertension as the only co-morbid factor commenced independent walking earlier than their counterparts who were both hypertensive and diabetic. The neurological outcome of stroke has been observed to be poorer in patients with diabetes than those without diabetes [4], thus suggesting that occurrence of diabetes mellitus as a co-morbid factor in stroke patients may prolong functional recovery in stroke. A stroke patient who has associated diabetes mellitus especially with complication such as peripheral polyneuropathy, which causes tingling sensation and numbness in the feet, may not be motivated to practice standing which is a prerequisite to walking.
Level of disability of the subjects had a significantly negative influence on the time they commenced independent walking in this study. The trend was such that subjects with mild disability at baseline commenced independent walking earlier (4.00 ±0.01 weeks) than those with moderate disability (7.72 ± 2.53 weeks). Initial disability would therefore be a negative influencing factor on recovery of independent walking by post stroke victims. A group of researchers[9] who observed that patients with mild and moderate disability had functional recovery within 2 months and 3 months respectively had concluded that the most important factor for functional recovery from stroke remains the initial severity of stroke.
Time of commencement of independent walking was not significantly different across the four personality types in these subjects. This suggests that their personality, a cognitive function, did not influence commencement of independent walking,although cognitive make-up had been observed to be one of the psychological factors that exert a major impact on patient’s rehabilitative functioning. Psychological adjustment was also reported to significantly enhance rehabilitation from a physical disability and a major contributing factor to the disability itself [7]. It is possible that other clinical and non-clinical factors modulated the potential influence of personality of the participants in this study. These include non-clinical factors like socio-cultural practice in this African community where the extended family practice ensures that a hospitalized stroke patient is surrounded by family caregivers. The regular presences of these family caregivers may serve as motivational factor that may dampen the likely influence of the patient’s own personality profile on recovery post stroke.
A major drawback of this study is the relatively small sample size. Also, although the participants received structured physiotherapy care, they were at different stage of recovery at the time of recruitment to the study. This could have contributed to some of the trends observed in this study.
CONCLUSION
The mean time for commencement of independent walking was 7.4 ± 2.6 weeks for all subjects and 4.00 ±0.01 weeks for those with mild disability at the point of recruitment into the study. Older age and a high score on the FIM scale generally characterized early commencement of independent walking.
| Acknowledgement |
| The authors would like to acknowledge all patients who participated in the study and the physiotherapists working at the department of physiotherapy, University College Hospital, Ibadan Nigeria for their cooperation during this study. The editorial assistance from Bisi Hamzat of Bital Consultancy Nigeria while preparing this manuscript is also acknowledged. |
Table 1: Mean Quantifiable Parameters of the Subjects (N=27)
| Variables |
range |
mean ± SD |
| Age (years) |
38.0 – 75.0 |
56.96 ± 10.49 |
| Years of education |
0.0 – 18.0 |
11.52 ± 5.93 |
| Admission-referral interval (Days) |
1.0 – 30.0 |
8.11 ± 6.58 |
| Functional Independence measure |
60.0 – 94.0 |
76.63 ± 7.88 |
| Independent walking attainment time (days) |
4.0 – 14.0 |
7.44 ± 2.61 |
Table 2: Comparison of the Mean Independent Walking Attainment Time by Clinical Factors Using Mann-Whitney U (N = 27).
| Variable |
Mean ± SD |
U-Value |
p |
| Sex |
|
|
|
| Male (n = 14) |
7.00 ± 2.54 |
73.00 |
0.38 |
| Female (n = 13) |
7.92 ± 2.81 |
|
|
| Side of affectation |
|
|
|
| Right (n = 17) |
7.47 ± 2.37 |
72.00 |
0.64 |
| Left (n = 10) |
7.40 ± 3.13 |
|
|
| Co-morbid factor |
|
|
|
| HTN (n = 21) |
7.00 ± 2.28 |
40.50 |
0.18 |
| HTN + DM (n = 6) |
9.00 ± 3.35 |
|
|
|
| Level of disability |
|
|
|
| Mild (n = 2) |
4.00 ± 0.001 |
1.00 |
0.03* |
| Moderate (n = 25) |
7.72 ± 2.53 |
|
|
Key: * = significant U at p ≤ 0.05, HTN = hypertension, DM = Diabetes Mellitus
Table 3 Comparison of the Mean Independent Walking Attainment Time by Psychosocial Factors Using Kruskal Wallis K (N = 27).
| Variable |
Mean ± SD |
K-value |
p |
| Personality types |
|
|
|
| Psychotic (n = 8) |
8.57 ± 3.20 |
|
|
| Neurotic (n = 10) |
7.25 ± 2.26 |
2.57 |
0.46 |
| Extrovert (n = 6) |
6.40 ± 3.29 |
|
|
| Introvert (n = 3) |
7.33 ± 1.15 |
|
|
| Level of education |
|
|
|
| None (n = 2) |
5.00 ±1.41 |
|
|
| Primary (n = 8) |
8.38 ±2.83 |
4.62 |
0.20 |
| Secondary (n = 5) |
8.40 ± 2.70 |
|
|
| Tertiary (n = 12) |
6.83 ± 2.41 |
|
|
| Occupation |
|
|
|
| Trading (n = 10) |
8.10 ± 3.35 |
|
|
| Civil-servant (n= 7) |
6.86 ± 2.91 |
2.32 |
0.51 |
| Retired (n = 6) |
6.50 ± 1.22 |
|
|
| Artisans (n = 4) |
8.25 ±1.26 |
|
|
| Marital status |
|
|
|
| Single (n = 0) |
0.00 |
|
|
| Married (n = 22) |
7.18 ± 2.34 |
2.40 |
0.30 |
| Separated (n = 2) |
11.00 ± 4.24 |
|
|
| Widowed (n = 3) |
7.00 ± 3.00 |
|
|
Table 4: Correlation between Independent Walking Attainment Time and Age, Years of education, Admission-Referral Interval and F.I.M score.
| Variables |
r – value |
p – value |
| Age |
– 0.57 |
0.00* |
| Years of education |
– 0.08 |
0.71 |
| Admission-referral interval |
0.02 |
0.91 |
| Functional independence measure |
– 0.55 |
0.00* |
Key: * = significant r at p ≤ 0.05
WORLD FEDERATION OF NEUROLOGY EDUCATION PROGRAMMESCME Programme
This programme is open to neurological societies that are members of the WFN and also from low or middle income countries as specified by the World Bank. At present, 38 societies participate in the programme each with a coordinator responsible for its local organisation.
Societies receive two mailings a year in January and July, of the series Continuum, which are generously donated to us by the American Academy of Neurology. In order to enhance the effectiveness of these courses the programme incorporates a discussion group format. Mailing costs are paid for by the WFN.
There will be new arrangements in the next few months when Continuum is to be made available free of charge to members on line. These may include a facility whereby individual neurologists, unable to attend discussion groups, can access Continuum from a location convenient to them.
Book Sharing Programme
Established in 2003, this programme links together individuals, neurologic departments, and publishers in resource-rich countries with those in need of neurological information elsewhere in the world. The programme now has 29 members worldwide receiving donations from individual neurologists and publishers.
Recipients must be neurologists who are coordinators of the WFN CME Programme, heads of departments or training programs, or their designees, and live in countries listed as “low” or “middle income” by the World Bank. Donors are put in touch with recipients by the WFN, establish email contact, arrange delivery of the books/journals/CD-ROMs on offer, and accept responsibility for shipping and shipping costs. Publishers also offer significant numbers of books and ship these books to the WFN’s storage facility for distribution.
To be considered as a member of either the CME or Book Programme, or to offer a donation to the latter, please email either Dr Theodore Munsat, Director, (Theodore.Munsat[at]tufts.edu) or Monica Brough, Programme Manager, at Monica.Brough[at]btopenworld.com.
PROVERBS / PROVERBES
– Do not vacillate or you will be left in between doing something, having something and being nothing.
– Le mensonge donne des fleurs mais pas de fruits.
– Lorsque tu ne sais pas où tu vas, regarde d’où tu viens. |
| |
PRE-CONGRESS SEMINAR ON MOVEMENT DISORDERS
Pan African Association of Neurological Sciences
Association Pan Africaine des Sciences Neurologiques
XVIIth PAANS Congress, Lagos, Nigeria, August 8 – 11, 2006
Pre-congress Seminar on Movement Disorders
8th August 2006
The Scientific Programme committee of the XVIIth Congress of the Pan African Association of Neurological Sciences hereby announces that a pre-congress seminar on Movement Disorders will take place as part of the pre-congress educational programme. The seminar will hold on the 8th of August, 2006, in the Seminar Room of the Department of Medicine, College of Medicine / Lagos University Teaching Hospital, Idi araba, Lagos.
Objectives: The purpose of the seminar is to update neurologists and other neuroscientists on the current diagnostic evaluation and management of various movement disorders. Emphasis will be placed on neurogenetics, clinical diagnostic criteria, and treatment modalities available in the African region.
Resource persons: The seminar will be facilitated by Dr. Jim Bower from the Movement Disorders Unit, Mayo Clinic, Rochester, Minnesota, USA, and Dr. Jonathan Carr from South Africa.
Course content: The seminar will be a one-day programme comprising of lectures, interactive sessions, and video demonstrations of various movement disorders. The topics to be covered include an overview of movement disorders, parkinsonian syndromes, tremors and myoclonus, dystonias, chorea, and interesting gait disorders.
Registration: The seminar registration fee is US$50 (N7000) for fellows and faculty, and US$40 (N5000) for trainees. Trainees must provide letters from their institution of training or appropriate institutional identification as proof of their status. Interested participants should send a notification of intention to attend via e-mail, including the following: full names, title, status (trainee, attending physician/consultant, medical officer, etc), institution and affiliation, contact address, to the e-mail address provided below. The e-mail message should be captioned “PAANS Movement Disorders Seminar”. The deadline for registration is 15th July 2006, while the deadline for payment is 31st July 2006. In special circumstances, payment may be made onsite (following receipt of notification of intention to attend by the deadline). Acceptance for the seminar is on first-come first-served’ basis and confirmation of registration will be done only after receipt of payment.
Method of payment: Payment of fees must accompany the notification of interest. Payment can be made by the following methods: bank certified cheques, bank drafts and or international money order should be in Nigerian Naira (Nigerian delegates only) or US$ and made payable to PAANS 2006.
Transportation and Accommodation. Please see the general announcement for the main conference. The Department of Medicine, College of Medicine, Idi Araba, Lagos, venue of the seminar, is 30 and 45 minutes by car from the domestic and international airports respectively.
Applications and payment should be sent to: Dr. Njide Okubadejo, Department of Medicine, College of Medicine/Lagos University Teaching Hospita, Idi-Araba, Lagos, Nigeria.
Professor M. T. Shokunbi
Chairman, Scientific Programme Committee, PAANS 2006
Department of Neurological Surgery, Institute of Neurological Sciences
University College Hospital, PMB 5116,
Ibadan, Nigeria
e-mail: paans2006@yahoo.com
Tel: +234-802-291-2220