
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
RESUME Introduction But Méthode Résultats Conclusion Mots clés : hydrocéphalie, ventriculo-cisternosmie, complication ABSTRACT Introduction Aim Method Result Conclusion Keys words: hydrocephalus, ventriculostomy complication INTRODUCTION La ventriculo-cisternostomie (VCS) représente une technique endoscopique de traitement de l’hydrocéphalie rentrant dans le cadre de la neurochirurgie mini-invasive [36]. Elle a l’avantage d’être simple, d’éviter les risques infectieux et mécaniques liés à l’implantation d’une valve, ainsi que de rétablir une circulation du liquide céphalo-spinal (LCS) proche de la normale. Elle peut néanmoins être émaillée de diverses complications qui sont quelques fois fatales [4, 33,34]. Nous analysons les différentes complications liées à la réalisation de la VCS chez 155 patients pris en charge pour hydrocéphalie. METHODOLOGIE RESULTATS Nous avons répertorié 167 patients ayant bénéficié d’une VCS dont 155 disposaient de toutes les données nécessaires à cette étude. Ceux ayant présenté des complications étaient 42 soit 27,1%. Il y avait une prédominance masculine (25 patients) avec un sex-ratio de 1,47. La tranche d’âge la plus représentative était celle des moins de 6 mois (24.5%) avec une moyenne d’âge de 10 ans (119 mois) et des extrêmes de 2 mois et 68 ans (876 mois). L’hydrocéphalie était causée par une sténose de l’aqueduc dans 22 cas, une malformation de Dandy Walter dans 6 cas, post-méningitique dans 5 cas, une tumeur de la fosse cérébrale postérieure dans 5 cas, une tumeur pinéale dans 3 cas et un kyste du V3 dans 1 cas (fig.1). Nous avons recensé 15 patients chez qui la VCS a été abandonnée en per opératoire (9.7%) pour diverses raisons (fig.2). Complications per opératoires Les saignements sont survenus chez 4 patients soit 2.6%. Ils étaient essentiellement liés à une blessure des plexus choroïdes (1 cas), une lésion des veines cortico-durales (1 cas) et non précisés pour les 2 cas restants. Ces saignements étaient de moyenne abondance. Complications post opératoires La fuite du LCS était retrouvée dans 15 cas soit 9,68%. L’âge des patients variait de 2 mois à 38 ans avec une moyenne de 10.56 ans. Les étiologies retrouvées étaient : 3 cas de sténose de l’aqueduc de Sylvius, 6 cas de Dandy Walker, 4 cas de tumeur de la FCP, 1 cas post-méningite et une tumeur de la région pinéale. Le délai moyen de survenue était de 14.5 jours. La prise en charge a consisté à une suture secondaire chez 9 patients dont l’un a bénéficié en plus d’une antibiothérapie. Une dérivation ventriculo-péritonéale (DVP) a été réalisée chez 2 patients, et une dérivation ventriculo-externe (DVE) chez 3 patients. L’infection a concerné 7 patients soit 4,52%. Il s’agissait de la méningite dans 6 cas avec un délai moyen de survenue de 25,5 jours secondaire à une fuite du LCS dans 1 cas, et liée à un manque d’asepsie au cours des soins prodigués aux patients dans les suites post-opératoires dans 5 cas. L’âge des patients variait de 4 mois à 35 ans avec une moyenne de 8.52 ans. Les étiologies de l’hydrocéphalie étaient la sténose de l’aqueduc de Sylvius dans 3 cas, 1 cas post méningitique, une tumeur kystique du V3 dans 1 cas et une tumeur de la région pinéale. Le délai moyen de survenue était 25.5 jours. La prise en charge de ces patients a consisté à une antibiothérapie adaptée, et à la pose d’une DVE chez un patient et d’une DVP chez un autre. Une suppuration de plaie opératoire a été constatée chez une patiente âgée de 11ans, porteuse d’une sténose de l’aqueduc de Sylvius après un délai de 6 jours. Elle a été traitée par antibiothérapie (céphalosporine de 3ème génération) associée aux soins locaux. Un patient de 11 mois, porteur d’une hydrocéphalie post méningitique a présenté une hyperthermie à 38°7 un jour après son opération sans signe clinique ni bactériologique de méningite. Il avait bénéficié d’un traitement symptomatique à base d’un antipyrétique. L’évolution était favorable. Un cas de diabète insipide avait été diagnostiqué chez une femme de 68 ans porteuse d’une sténose de l’aqueduc de Sylvius 2 jours après son intervention. La symptomatologie a régressé après un traitement médical. Un échec de la VCS a été rapporté dans 11 cas soit 7,1% dont 7 patients de sexe masculin. L’âge des patients variait de 5 mois à 25 ans, avec une moyenne de 8,1 ans. L’étiologie de l’hydrocéphalie était dominée par la sténose de l’aqueduc de Sylvius (8 patients). Le délai moyen de survenue était de 6.56 mois. Une DVP secondaire a été faite pour 9 d’entre eux, une reprise de la VCS pour 1 et une abstention thérapeutique dans 1 cas. Une obstruction secondaire a été notée chez 2 patients âgés de 3 et 4 mois. Les étiologies retrouvées étaient une malformation de sténose de l’aqueduc de Sylvius et une tumeur de da FCP. Le délai moyen de survenue était de 12 mois. La prise en charge a été une DVP et une reprise de la VCS, avec une évolution favorable dans 1 cas (celui de la DVP). Nous avions enregistré au cours de cette étude 2 décès soit 1,29%. Le premier patient âgé de 30 ans, porteur d’une sténose de l’aqueduc de Sylvius, était décédé au 3ème jour postopératoire suite à une hémorragie non contrôlée. Le second patient âgé de 4 ans, avait développé une méningite suite à une fuite du LCS et est décédé au 34ème jour. DISCUSSION Considérée comme une alternative à la dérivation du LCS (shunt), la VCS est le traitement de choix des hydrocéphalies obstructives ; cependant elle peut être émaillée de certaines complications. Sur 155 patients traités, 42 ont présenté des complications soit 27,1%. Ce taux se rapproche de celui de Proust : 26% [29] et d’Ersahin : 25% [9]. Selon certains auteurs, le taux de complication de procédures endoscopiques varie de 0 à 20% [7,33]. La sténose de l’aqueduc de Sylvius représente l’étiologie de l’hydrocéphalie la plus fréquemment retrouvée au cours de notre étude : 52,4% des complications. Ersahin et al [9] par contre ont retrouvé un taux de complication important chez les patients ayant une obstruction du 4ème ventricule (V4) (68%) et moindre chez ceux ayant une malformation de Chiari type I et une tumeur. Le taux de complication durant notre étude a été plus important au cours de la 2ème année de la pratique, et décroissant sur le reste de la période. Ceci a été également rapporté par différentes équipes [8,25] et s’expliquerait par l’accroissement de la maitrise de la technique par les chirurgiens : il s’agit de la courbe d’apprentissage de la procédure neuroendoscopique. Le taux d’abandon de notre étude (9,68%) est dans les limites rapportées par la littérature : 0 à 26% [5,39]. Les raisons d’abandon étaient essentiellement l’hémorragie et les variations anatomiques tel le cloisonnement du foramen de Monro. Complications per operatoires La principale complication peropératoire rencontrée était le saignement (2,58%). Il représentait 0,53% au cours de l’étude de Schroeder [33] et 2,9% au cours de celle de Sokal [36]. L’hémorragie intraventriculaire émanant des petits vaisseaux sous-épendymaires par impact des instruments endoscopiques est la plus fréquemment rapportée [5,12]. L’hémostase a été obtenue comme l’a suggéré Walker [41]: irrigation et patience dans 2 cas. Pour les 2 autres, le recours à la DVP a été indispensable. Le pronostic était défavorable chez un patient. Nous n’avons pas eu de cas de saignement de gros vaisseaux. Pour la plupart des auteurs, les lésions des gros vaisseaux sont rares et représentent environ 1% des VCS [21,33]. Complications post operatoires La fuite du LCS a concerné 15 de nos patients soit 9,68% et est la complication la plus fréquente au cours de notre étude comme lors de celles de plusieurs autres auteurs [30,33, 40] et peut mener à une ventriculite ou une méningite [28]. Une fuite ou un épanchement sous-cutané du LCS signe un échec [9]. Une augmentation de la pression intracrânienne se traduisant par une fuite du LCS peut survenir dans la période postopératoire précoce car la restauration du mécanisme de résorption des granulations arachnoïdiennes n’est pas immédiate, il faudra pour cela un temps d’adaptation [3,26]. Des ponctions lombaires sont nécessaires durant cet intervalle. Kombogiorgas et Sgouros [19] pensent que la fuite du LCS dans la période postopératoire immédiate est au contraire associée à une réussite de la VCS. La prise en charge de nos patients a été dominée par la suture secondaire de la plaie opératoire associée à des ponctions lombaires déplétives. L’infection a concerné 7 patients soit 4,52%. Schroeder et al [34] ont rapporté un cas de suppuration de plaie ayant entrainé une méningite puis un décès par défaillance multi viscérale 4 semaines après la procédure. Sanoussi et al [31] sur 144 patients ayant bénéficié d’une VCS n’ont rapporté aucun cas d’infection. Un patient a développé un diabète insipide qui a été pris en charge avec une évolution favorable. Cette situation pourrait être liée à un traumatisme de la tige pituitaire. Di Rocco et al [7] quant à eux, ont rapporté le cas d’un enfant de 2 ans porteur d’une malformation de Dandy Walker ayant eu un diabète insipide définitif après VCS. L’échec de la procédure a été constaté dans 11 cas (7,1%). Selon Yadav [43], on parle d’échec de la VCS quand il y a une persistance de la symptomatologie ou une progression de la dilatation ventriculaire avec une pression intracrânienne élevée. L’hydrocéphalie est dans ces cas la résultante d’une obstruction de la circulation et d’une absorption défectueuse du LCS : on parle alors d’hydrocéphalie complexe. L’incidence est beaucoup plus élevée chez les patients ayant eu une méningite tuberculeuse. Elle est une cause d’échec de la VCS [43]. Pour certains auteurs le risque d’échec est important, particulièrement chez les enfants de moins d’un an [8,30]. Selon Javadpour [15] et Fritsch [11] l’âge n’est pas une contre-indication ni un facteur de risque opératoire. La réussite de la VCS est plutôt fonction de la cause de l’hydrocéphalie. L’étiologie de l’hydrocéphalie la plus retrouvée pour les échecs durant notre étude était la sténose de l’aqueduc de Sylvius (8 cas). Elle va à l’encontre des données de la littérature selon lesquelles la sténose de l’aqueduc de Sylvius serait l’étiologie qui aurait le meilleur taux de réussite atteignant 90% [2,27]. Pour Cinalli et al [6] la plupart des échecs surviennent chez des patients porteurs d’une myeloméningocèle et d’une malformation de Chiari de type I au cours desquelles une masse intermédiaire peut cacher le plancher du V3, et chez les patients ayant souffert d’une ventriculite, car les repères anatomiques deviennent méconnaissables. Nous pourrions expliquer notre constat par le fait que la sténose de l’aqueduc de Sylvius est plus souvent observée chez les enfants. La prise en charge secondaire a consisté essentiellement à la réalisation d’une DVP. Celle-ci doit être faite chez les patients qui ont une stomie patente et une persistance de la pression intracrânienne au delà de 10 à 15 jours après 3 à 5 ponctions lombaires [44]. Les auteurs coréens [37] préconisent l’implantation simultanée d’un drain ventriculo-péritonéal et la réalisation d’une VCS comme premier choix de traitement de l’hydrocéphalie chez les patients de moins d’un an. Le cathéter ventriculaire doit être placé au niveau de citerne pré-pontine sous guidage endoscopique réduisant ainsi le risque de sténose secondaire par développement de nouvelles membranes arachnoïdiennes. Ils ont rapporté 83,9% de réussite. On note un seul cas de reprise de VCS. Balthasar et al [1] préconisent en cas d’échec, de tenter d’abord une seconde VCS avant de poser un shunt chez les jeunes enfants, car le taux de réussite de la VCS augmente rapidement 4 mois après la naissance. L’échec précoce peut être lié à un dysfonctionnement du système d’absorption du LCS, soit par immaturité ou soit par défaillance [8,30]. Quant à l’échec tardif, il est lié à l’obstruction de la stomie [9] et varie de 2 à 15% à travers la littérature [8,10]. L’hydrocéphalie obstructive chez les patients très jeunes est généralement une combinaison de problème obstructif et d’absorption [44]. Contrairement à Cinalli et al [6] qui ont rapporté 11 cas (4,7%) d’hygromes sous-duraux, nous n’en avons rapporté qu’un seul soit 0,65%. Le mécanisme physiopathologique associerait une décroissance brutale du volume ventriculaire induite par un drainage brusque lors de la VCS et la traction du parenchyme du lobe frontal chez les patients qui ont déjà un manteau cortical mince [35]. La fenestration de kyste arachnoïdien chez les nouveau-nés est le geste le plus incriminé dans la survenue alors qu’il n’en était pas le cas chez notre patient âgé de 4 ans. Daprès Schroeder [33], les collections sous-durales sont beaucoup plus fréquentes lors de la dérivation ventriculo-péritonéale que lors des VCS. Comme Ersahin et al [9], nous avons rapporté 2 cas de sténose secondaire de la stomie due probablement à la formation de nouvelles membranes arachnoïdiennes ou une cicatrisation. Une VCS répétitive a été faite avec succès chez un, dans leur cas. Nous avons opté dans un cas à une DVP et dans l’autre cas à une VCS. Selon Mohanty et al [23] une sténose secondaire de la stomie par gliose ou cicatrice est responsable de 6 à 15% des échecs de la VCS. Il représente 4,76% des échecs pour notre étude. Kadrian et al [17] ont rapporté des pourcentages de patients « présumés avoir une VCS fonctionnelle après 5 ans » comme suit : 41% chez des patients âgés de 1 à 6 mois au moment de l’intervention, 58% chez les patients âgés de 6 à 24 mois, et plus de 70% chez les patients âgés de plus de 24 mois. Ces résultats correspondent à ceux des autres auteurs [18]. D’autres complications ont été décrites mais non retrouvées dans notre série telles : une altération transitoire de la mémoire, des troubles du rythme cardiaque, une compartimentalisation secondaire, un syndrome d’amnésie antérograde associé à une boulimie; un désordre de la personnalité; un infarctus frontal, un hématome sous dural aigu…[9]. Schroeder et al [33] recommandent pour minimiser les complications que la stomie soit faite à mi-distance entre les récessus infundibulaires et les corps mamillaires sur la ligne médiane. Ainsi la perforation est localisée juste derrière le dorsum sellae. Nous avons déploré 2 cas de décès (1,29 %). Ce taux concorde avec certaines données de la littérature [29,33]. Pour d’autres auteurs [33,38], le taux de mortalité est généralement inferieur à 1% et la mort survient après un saignement catastrophique des gros vaisseaux ou soit par arrêt cardiaque per opératoire [21] due à une soudaine augmentation de la pression intracrânienne lors d’une irrigation rapide. Le décès peut aussi survenir longtemps en moyenne 7 ans après la stomie [14] mais le risque est faible [16]. L’examen autopsique dans ces cas révèle une présence de prolifération gliale et de cicatrice confirmant la sténose d’où l’hypertension intracrânienne aigue expliquant le décès [13]. Pour réduire le taux de mortalité associé à un échec de VCS, Mobbs et al [22] ont suggéré de laisser un cathéter ventriculaire et un réservoir sous-cutané à la fin de l’intervention pour permettre des procédures d’urgence en cas de nécessité. L’association échec de la VCS et mort subite ne serait pas seulement liée à la technique mais au profil des patients (hydrocéphalie obstructive). Ces patients sont en fait enclin à une détérioration clinique soudaine, et des épisodes similaires ont été décrites même quand ils sont uniquement traités par DVP lors d’un dysfonctionnement [28,20]. La plus grande étude portant sur les succès de la VCS a été faite en Ouganda et concernait 153 patients âgés de moins de un an. Le taux de succès au sein de cette population était de 53%. Le taux de réussite de la chirurgie chez les patients ayant une myeloméningocele est de 40% contre 70% pour ceux ayant une obstruction aqueducale [42]. CONCLUSION Les complications relatives à la VCS sont non négligeables, dominées par la fuite du LCS et fonction de l’expérience du chirurgien. La sténose de l’aqueduc de Sylvius est l’étiologie dominante de l’hydrocéphalie des complications au cours de notre étude. Un suivi postopératoire rigoureux et une technique bien maitrisée est indispensable pour minimiser les complications.
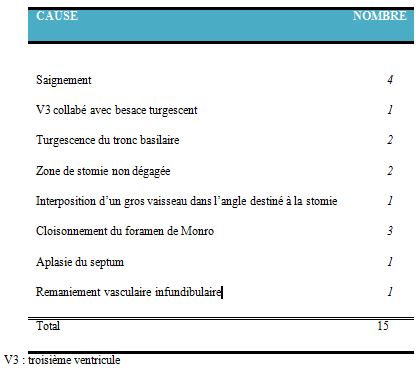 Figure 2 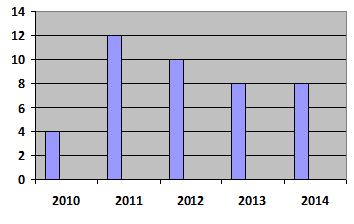 Figure 3 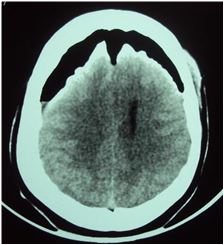 Figure 4 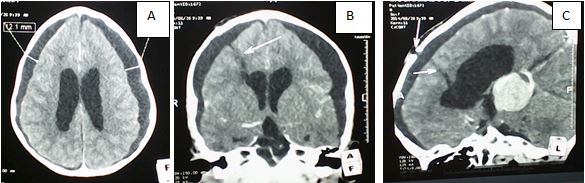 Figure 5
ABSTRACT Background and objective: Methods Results Conclusion Keywords: parasuicide, craniocerebral injury, gunshot wound INTRODUCTION Civilian craniocerebral gunshot injuries (CGIs) result in severe traumatic brain injury, forming a significant public health affliction in South Africa (SA) and internationally [7, 12, 16]. The underlying aetiology of self-inflicted gunshot head injuries (SIGHI) following suicidal intent (SI) is multi-factorial. SA has a substantial history of violent trauma, fuelled by social strife and easy access to firearms [9, 13, 14]. Furthermore, recent reports suggest that SA has the 22nd highest suicide rate worldwide, with guns contributing to this phenomenon [4, 14]. SIGHIs impart a high pre-hospital mortality due to their destructive nature [1, 10, 12, 15, 18, 19]. A patient receiving treatment at a neurosurgical unit (NU) following this type of injury, thus offers a unique opportunity to gain insight into a survivor. Furthermore, in SA, there is paucity of data on management of these types of injuries, with most reports based on post mortem studies [2]. The purpose of the current study was to report the prevalence, demographics and characteristics of these cranial injuries with regards to presentation, radiological findings, management, and outcomes at the NU in Inkosi Albert Luthuli Hospital (IALCH) which is well suited; being the only public neurosurgical service in the province of KwaZulu-Natal (KZN), catering to a population of over 10 million people [5]. METHODS This was a retrospective, observational, descriptive study performed at a single institution. We reviewed medical records of patients treated in the NU at IALCH with a diagnosis of a CGI during January 2003 to September 2014. From this cohort of patients we selected and included into the study sample those with a diagnosis of SIGHIs following SI. Those patients who were victims of inter-personal violence and those with accidentally-inflicted gunshot head injuries were excluded. The study approval was granted by the Biomedical Research Ethics Committee of the University of KwaZulu-Natal (reference number BE007/14). Variables investigated included age, gender, neurological deficit, Glasgow Coma Scale (GCS) on admission and discharge, gunshot entry point, computerised tomography (CT) findings, management, complications, length of hospital stay (LOS), and in-patient mortality. Data was collected using a data collection sheet, captured in Excel® (Microsoft Inc., WA, USA) and analysed using Stata® version 14 (StatCorp LP, Texas, USA). Means (with standard deviations), medians and frequencies were used to describe the data. The Wilcoxon Mann-Whitney test was used to compare continuous variables between subgroups. Associations between categorical variables were tested using the Fisher’s exact test. Results with a P-value of <0.05 was considered statistically significant. Management of patients with CGIs in the NU at IALCH is guided by the ATLS® principles [6], followed by an urgent computerised tomography (CT) brain scan as a form of investigation. Angiography is performed if a vascular injury is suspected. Upon reviewing these investigations, patients are taken for operative management, which is based on the Brain Trauma Foundation guidelines [3] and the management principles of gunshot head wounds [1, 10, 12, 16, 18]. Tetanus toxoid is administered at admission whilst a course of empiric antibiotic therapy with gram positive cover is commenced and continued post-operatively for 7-days. Anti-seizure prophylaxis is routinely administered for 7 days post-injury and discontinued if seizures are not documented during this period. RESULTS A total of 499 patients with the diagnosis of a CGI were identified during the study period. Thirty-one (6%) of these patients were survivors of SIGHIs following suicidal intent. Table 1 demonstrates their clinical characteristics. Majority of patients were male [28; 90%], with a male-to-female ratio of 9:1. The gunshot wound entry sites are shown in Table 2. The clinical presentations included hemiplegia [6; 19%], pupillary abnormality [2; 6%], facial palsy [2; 6%], visual loss [2; 6%], cerebrospinal fluid (CSF) otorrhea [1; 3%], and seizures [1; 3%]. The CT brain scan findings and missile injury morphology are shown in Table 3. CT Angiography in one patient revealed a traumatic right middle cerebral artery (MCA) pseudoaneurysm (Figure 1). All patients were managed surgically and the procedures performed were wound debridement craniectomy [19; 61%], superficial wound debridement and closure [7; 23%], craniotomy [4; 13%] and decompressive craniectomy [1; 3%]. Six (19%) patients required neurocritical care which included intracranial pressure (ICP) monitoring and ventilation. Eleven (35%) patients developed early post-operative cranial complications. Septic morbidity occurring in ten (32%) patients comprised the majority of these cases and was due to meningitis [6; 19%], wound sepsis [4; 13%], and intracerebral abscesses [3; 10%]. The microbes responsible for these infective complications were acinetobacter baumani (2), staphylococcus aureus (1), and pseudomonas aeruginosa (1); with five patients not yielding an offending organism. Management of wound sepsis and intracerebral abscess included surgical debridement and excision of the abscesses in operating theatre, followed by directed antibiotic therapy guided by microscopy, culture and sensitivity results. Seven patients (23%) had CSF fistulae; with five of them developing meningitis. The CSF fistulae presented as rhinorrhea [3; 10%], otorrhea [1; 3%], contained pseudomeningocele of the scalp [2; 6%], and an open wound leak [1; 3%]. Seven (23%) patients with SIGHIs demised during the study period and they had a significantly lower post resuscitation GCS ≤ 8 (P = 0.018) and age ≥ 39 years (P = 0.026). Four (22%) of the eighteen patients that sustained transaxial injuries demised, yet this did not show a statistically significant contribution to mortality (P = 0.999). DISCUSSION SIGHIs impart destructive injuries following maximal energy transmission to the brain due to the close range of the weapon. Survivors of SIGHIs provide a small proportion to the overall CGIs in our unit when compared to the experience of other centres [11]. This could partially be explained by the particularly high pre-hospital mortality, and with our centre being the only NU in the province, delays in transfer further influence the number of salvageable survivors making it to the unit. Also, firearm legislature and socioeconomic factors vary between countries, affecting gun usage and resulting in differing patterns of CGIs. Suicide attempts are reported to be more common in females and young adults [17]. Females though are less likely to possess firearms and use them in suicide attempts. Victims of such injuries are frequently reported to be males [19], and this has been mirrored in our study. The predominance of males and the median age in the current study fall within a similar range to victims of traumatic brain injury following interpersonal violence treated in our unit [8]. The underlying factors leading to SI are many, amongst them being work related stress, depression, relationship discontent, alcohol and drug abuse. The admission post-resuscitation GCS has been reproduced in numerous studies as the single strongest clinical predictor of outcome in gunshot head injuries [1, 7, 16, 18]. Our findings did suggest that patients presenting in coma (post-resuscitation GCS ≤ 8) are more prone to mortality. A CT brain scan is a vital investigative tool in the acute management of these patients. It displays the injury morphology, is used to plan surgical intervention, and used as a baseline for follow-up. It can also be used to prognosticate the injury, as presence of tranventricular and bihemispheric injury is associated with a poor outcome [1, 16]. Transaxial CGIs though known to be associated with high mortality did not show a statistical significant relationship to mortality in our study [16]. This atypical finding could be explained by the small patient numbers and that majority of these injuries were bifrontal, possibly not affecting absolute critical structures in the brain. Regarding the entrance site, the frontal regions predominated and together with the temporal area formed the majority of the sites of injury, which is congruent with the possible gun orientation during a suicide attempt [2]. Furthermore, with self-inflicted close range gun orientation leaving little room for error, it is not unsurprising that a tangential injury would not be likely and was the least common type of gunshot head wound in our series. Angiography is an ancillary imaging modality employed in those where there is concern of significant neurovascular injury. A middle cerebral artery pseudoaneurysm was discovered in one patient. The said individual had a heavy subarachnoid blood load in the sylvian fissure adjacent to the bullet tract and CT hypodensities suspicious of ischaemia, which prompted this further investigation. However, this patient had a GCS of 6 and was deemed a poor grade for intervention. Emergent surgical management via a craniotomy or craniectomy is life saving in patients with intracranial haematomas causing raised intracranial pressure. Surgical debridement involves removal of necrotic brain tissue, loose bone fragments and retained missiles when they are easily accessible. This is followed by repair of the dura in order to prevent post-operative CSF leaks. Infective complications remain a problematic cause of morbidity and mortality with CSF fistulae greatly increasing this risk; reaffirming the value of the operative debridement and dural repair as a vital component in this regard [11]. Every means of reducing septic sequelae should be adhered to, thus during the post-operative period judicious use of antibiotics is practiced [16]. Unfortunately, septic complications still occurred in 32% of our patients, which was higher than the rate reported by other authors [11]. An early post traumatic seizure occurred in one (3%) patient while admitted in the NU. These have been reported between 1.3% and 24% of CGIs [11], lending support to our protocol practiced for seizure prophylaxis. The mortality rate in our study of 23 % was within the reported range in other series [11]. Key to reducing the incidence of SIGHIs in SA lies in prevention strategies. This may involve identifying those at risk and intervening early through primary preventative psychosocial interventions, coupled with stricter gun control legislation to limit access to firearms. The limitations of this study are its retrospective nature, a small sample size, and no long-term follow-up. The study only analysed patients within the public health sector and those patients treated in the private sector have not been represented in our numbers. However, the study represents the experience of a single NU centre in KZN and thus gives us insight into the presentation and outcomes of survivors of SIGHIs who receive treatment at our institution. CONCLUSION Survivors of SIGHIs following an attempt at suicide account for a small contribution to the total CGIs in our practice. Early surgical treatment is critical in providing the best chances for a favorable outcome in those patients that survive the initial onslaught. Unfortunately though, those presenting in coma have poor outcomes. Holistic patient care involving a multidisciplinary team which includes rehabilitation specialists, social workers and psychologists is essential if these patients are to be re-integrated into society. However, due to constrained resources in our environment, this rehabilitative and psychological component is entrusted to step-down facilities upon discharge. To our knowledge this study is the first neurosurgical review of SIGHIs describing patient presentation and outcomes in KZN. This information can be useful in exploring the burden imparted on resources, may provide an impetus for preventative measures to be applied, assist in producing clinical recommendations, and help guide policies to institute more holistic patient management. CONFLICT OF INTEREST The authors declare no conflicts of interest. FUNDING SOURCE None EVALUATION AND MODIFICATION OF KANG’S MRI METHOD OF GRADING CERVICAL SPINAL CANAL STENOSIS AMONG AFRICAN PATIENTS: AN INITIAL STUDY.ABSTRACT Background Objective Materials and methods Results Keywords: Cervical Stenosis, Kang, MRI INTRODUCTION The size of the spinal canal and integrity of its content (mainly the cord) are the key prognosticating parameters that are considered when evaluating a patient for spinal disease. Cord compression could be developmental or degenerative and in adults, the commonest cause of cervical myelopathy is spondylosis.1, 2 The smaller diameter of the cervical canal leads to greater symptoms for relatively smaller degrees of stenosis than its lumbar equivalent. Earlier reports which attempted to assess cervical canal stenosis, started with cadarveric and radiographic studies.3-8 Plain radiographs are largely obsolete now because of inherent radiation risks, magnification errors and lack of soft tissue detail although CT it is still useful for osseous details. MRI on the other hand is the choice modality in assessing the spine, overcoming the radiographic limitations. Even with this superior modality, its use in diagnosing patients with cervical myelopathy has not been fully harmonized worldwide. Descriptive terminologies such as mild, moderate, severe stenosis 2, 9, 10, 11 are subjective, and vary in definition between different interpreters. Nagata et al12 and Harrop et al13 focused on the spinal cord but not the spinal canal while Muhle13 and Larsson11 considered the cord and canal but were silent about T2W signal intensity (SI) of the cord, which itself is a strong prognosticating factor for patients with cervical spondylotic myelopathy (CSM).1, 14-17 The Kang method was developed based on the preexisting method of Muhle, so as to allow for assessment of the canal, spinal cord and cord parenchymal changes. In Nigerian literature, we are not aware of any method of grading stenosis either using radiographic methods or MRI. This study to the best of our knowledge is the first MRI documentation on grading of cervical stenosis in our environment. It aimed to assess the reliability and adaptability of a modified Kang method in our practice; and to build a data base for future research. MATERIALS AND METHODS Case selection: Approval for this study was given by the hospital’s ethics committee. A total number of 140 patients were referred for cervical MRI scan during the two year period of this study. Out of these, MRI scans of 52 patients with cervical spondylosis were examined for this review. Our basis for exclusion included age ie < 16 years, post traumatic/surgery, spinal tumor/infection, and poor quality image. Our study population comprised of 36 males and 16 females. Their bio data and clinical history were obtained from patients' hospital records. Image acquisition Only one MRI machine (0.2Tesla MAGNETOM Concerto Siemens Medical) was used to image all patients. T1 and T2weighted images were acquired using the fast spin echo technique. Patients were imaged lying supine with the head in neutral position and the use of a neck coil. The imaging protocols were as follows:
Image analysis 2 experienced radiologists OAS and IPO with 8 years and 12 years’ experience respectively were presented with a schematic representation of the grading method (fig.1).10 The examiners were blind to the patients’ clinical information and MRI reports. Each examiner graded all 52 images at 4 cervical levels ie C3/4, 4/5, 5/6 and 6/7. Mid sagittal as well as immediate adjacent parasagittal images were studied in order to allow for grading to be done at the point of maximum compression. The examiners employed the method proposed by Kang (Fig.2) however grades were modified and classified as follows:
Statistical analysis Statistical analysis was done by SPSS version 20 (Chicago Illinois). Percentage inter-observer agreement among the 2 Radiologists was calculated using the kappa statistics. This was also calculated for sub categories among the 4 grades: for distinguishing between presence or absence of stenosis (grade 0 vs 1,2,3), between significant and non-significant stenosis (0,1 vs 2,3), and for presence or absence of cord injury ie T2W signal change within the cord (grades 0,1,2 vs grade 3). The agreement was then rated according to Landis and Koch19,. as follow: kappa values of 0-0.2 indicated slight agreement, 0.21-0.4 indicated fair agreement, 0.41-0.60 indicated moderate agreement, 0.61-0.8 indicated substantial agreement, and 0.81 or greater indicated excellent agreement RESULTS In this study, 52 patients were examined independently and they were made up of 36 (69.2%) males, 16 (30.7%) females. Age range was 36 years to 78 years old (mean age 56.1years SD 10.87years). For both examiners, grade 0 was the most prevalent grade scored as most patients had insignificant stenosis (grade 0, 1) Fig 6. The frequency of stenosis by cervical level is shown in Table 1. C6/7 level was least compressed (grade 0= 70%) while the level more severely affected (grade 3) was C3/4 followed by C5/6. The Inter observer agreement and kappa statistics for various distinctions in each level is shown in Table 2. The overall inter-observer agreement was high (k= 0.65 to 0.87). For most levels, the agreement was substantial to almost perfect except at the lowest cervical level. The distinction between the presence of stenosis, how significant, and the presence of cord injury was almost perfect at C3/4 levels (> 90%; k= 0.81 – 0.85), substantial to almost perfect at C4/5 (86.5-92.6%; k= 0.65 – 0.85) and C5/C6 (88.5-98.1%; k= 0.79-0.87 Table 3 shows analysis of symptoms with respect to distinction between the grades. Correlation was made between significance of stenosis ie grades 0, 1(insignificant) and 2, 3 (significant) versus neurologic symptoms. 22 (84.6%) of the 26 patients with significant stenosis had neurologic symptoms while 15(57.6%) of patients with non-significant stenosis did not have neurologic symptoms. DISCUSSION The need to standardize methods of assessing cervical stenosis has led to recent evolutionary studies. Larsson et al11 defined mild, moderate and severe stenosis to mean subarachnoid space obliteration less than 50%, greater than 50% and compression of the cord respectively while Muhle at al13 used a 4 point grading system where grade 0 meant normal, grade1 was partial obliteration, grade 2 was complete obliteration of anterior or posterior subarachnoid space, and grade 3 meant cord displacement or compression. Kang et al modified the Muhle classification in order to incorporate SI T2Weighted cord changes. The reliability of Kang method was assessed by Park et al20 while our presentation examined and modified the Kang study, with review of previous literature. We modified the original Kang grade 1 by subdividing into grades1a and 1b as follows:
Results from this study showed a significant level of agreement which is higher than the agreement in the original Kang study which ranged from 63%-64%. The improvement in the agreements is largely due to the fact that the observers in our study had both schematic and pictorial representations of the grading system before the patients were scored although they were blind to clinical information and MRI reports. In a study by Stafirra et al2 using CT and MRI in which they had no instructions or guidelines, there was significant disagreement among interpreters. Inter-observer agreement for level, degree and cause for CT myelogram was k= 0.5, 0.26, 0.32; for MRI k =0.6, 0.31, 0.22 Our study therefore supports the fact that the modified Kang system can be taught and be understood by Radiologists and managing Physicians. The prevalence of each grade did not differ significantly between the 2 readers in our study. We also assessed clinical value offered by the grading system by sub categorizing the grades. Grades 0 vs. 1, 2, 3 (absence vs. presence of stenosis), % agreement was almost perfect across C3-6 (>80%, k between 0.65 – 0.85) but moderate at C6/7 (80.8%, k=0.57). For grades 0, 1 vs. 2, 3 (non-significant vs. significant stenosis) % agreement was greater than 90% with k values of 0.81, 0.85, 0.87 respectively at C3-6 levels; and 0.38 at C6/7. While for 0, 1, 2 vs 3(presence of SI within the cord, the % agreement and k values were 98.1%, k=0.65, 92%, and 98.1%, k=0.79 and 98.1%, k=0.00 across C3/4 to C6/7 levels. These results show that agreement between the examiners were generally better at the C3-6 than at C6/7. The study by Kang only assessed 3 cervical levels and did not examine C6/7. Our results showed better agreements than Kang’s which recorded 81-85% ((0, 1 vs2, 3) and 91-95% (0, 1, 2 vs. 3). In the study by Park et al, they studied 4 cervical levels as we did but they had a slightly different modification from ours. In addition, they correlated their findings with clinical symptoms and neurologic examination. They however also recorded a higher prevalence of grade 0 similar to our report, unlike Kang who reported grade 1 to be the most prevalent grade. Again, this could be explained by the fact that in using older subjects (>60 years), Kang study would have fewer normal findings since spondylosis is mostly a process of aging. We also recorded that the cervical level least prone to compression was C6/7, which had the highest prevalence of grade 0. When we considered patients’ symptoms, most (22 out of the 26) patients with significant stenosis (grades 2 and 3) also had positive neurologic symptoms. All (100%) of patients with spinal cord injury, signified by high T2 signal intensity were found to have severe symptoms. However, patients’ symptoms compared less well with grades 0 and 1(insignificant stenosis). 42.3% of patients with non-significant stenosis had positive symptoms. But being a retrospective study, the severity of symptoms could not be assessed clinically. Our findings showed that out of 19 patients who were asymptomatic, 4 had severe stenosis and therefore we entertained the possibility of asymptomatic congenital stenosis. Our modification of Kang grade 1 into 1a and 1b did not lead to an upgrade or downgrade from the overall grading system and will not significantly affect the patients’ management in the short term. However, it conveys a relevant subtle clinical message of early onset stenosis. We believe that in our environment, the modified Kang will allow for surveillance of individuals who had mild stenosis and would otherwise be categorized as no stenosis (i.e grade 0) in the original Kang system. This is especially since we operate on a low field MRI machines in most parts of the country, and also because our patients were mostly much younger (less than 60 years), compared with the Kang study and with time their spondylotic process would increase as they get older. Patients with mild stenosis have been found to progress over time in previous reports. 21,22 CONCLUSION Our study is an initial preliminary retrospective study, a revised Kang scoring system (2016) and represents the first documentation in Nigeria. We agree that it is a method that can be taught and understood; and is reproducible on even low Tesla MR Scanners. Limitations The low field strength (0.2Tesla) scanner used may have affected image quality especially in axial plane (higher strengths were not available in our locality). Hence the use of only sagittal images where the delineation of the subarachnoid space and the spinal cord was clearer.
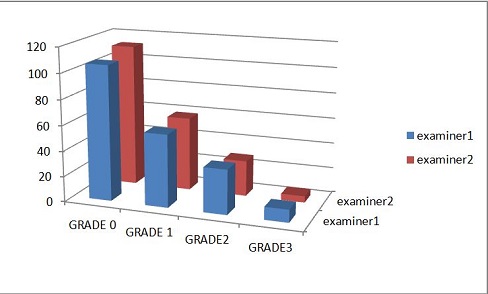 Figure 6 Table 1. The frequency of stenosis by cervical level
Table.2 The Interobserver agreement and kappa statistics for various sub categories of grades
Table. 3 Analysis of symptoms with respect to distinction between mild stenosis( ie grades 0 &1) and severe stenosis (grades 2 & 3)
RESUME Description Méthode Résultats La localisation droite était prédominante. Pour les techniques chirurgicales, l’abord sous- frontal était le plus utilisé (57,14%), l’étude histologique était en faveur des méningiomes dans 39,13% des cas. L’évolution était favorable avec une régression spectaculaire de l’exophtalmie et peu de morbidité. Conclusion Mots-clés : Abord sous frontal – Imagerie – Exophtalmie – Tumeurs orbitaires. INTRODUCTION Les tumeurs de l’orbite (TO) sont des tumeurs développées aux dépens de l’orbite et de son contenue (6). Nous entendons par TO non pas uniquement les tumeurs au sens anatomopathologique strict mais également les masses orbitaires de nature non tumorale. Bien que ces tumeurs soient rares, elles comportent une grande variété étiologique. Cependant la fréquence respective des différents types de lésions, varie de façon considérable selon que la série émane d’un service d’ophtalmologie, de neurochirurgie ou de groupe mixte (4). Le diagnostic est actuellement facilité par le développement des moyens d’investigations neuroradiologiques notamment l’imagerie par résonnance magnétique (IRM), et la tomodensitométrie crânio-orbitaire (TDM). L’histologie a permis de classer les entités dans des groupes relativement homogènes. Ces tumeurs deviennent neurochirurgicales lorsque la lésion occupe les deux tiers postérieurs de l’orbite. MATERIEL ET METHODE Ce travail a été basé sur l’étude rétrospective de 33 dossiers de TO pris en charge sur une période de 13 ans allant de 2002 à 2014, mais seuls 31 dossiers exploitables ont fait l’objet de cette étude. Les patients perdus de vue ont été exclus de notre étude. RESULTATS L’âge de nos patients était compris entre 2 et 50 ans, avec une prévalence élevée de la tranche d’âge de 21 à 40 ans (43,47%). L’âge moyen était de 26 ans. Les enfants (≤15 ans) représentent 30,43%. Il existe une prédominance féminine : 18 femmes (58,06%) contre 13 hommes (41,9%). Deux de nos malades avaient des antécédents de traumatisme oculaire (6%), dont un cas remontait à l’enfance et l’autre présentait un kyste orbitaire. Le délai de consultation variait entre 22 jours et 8 ans, avec une moyenne de 3 mois et demi. Le mode de début pour la majorité des cas était progressif (95,65%). L’imagerie a mis en évidence une prédominance de la localisation droite (56,52%). Un bilan d’extension a été demandé pour un seul cas (mélanome oculaire), se révélant négatif. La corticothérapie par voie générale a été instaurée initialement pour deux patients : un lymphangiome kystique et une pseudotumeur inflammatoire de la glande lacrymale biopsiés par les ophtalmologues. DISCUSSION Pathologie relativement rare, les tumeurs orbitaires se présentent cliniquement selon un tableau assez stéréotypé. Notre étude confirme le profil clinique et épidémiologique des TO. Le but de la neurochirurgie orbitaire, est d’éradiquer la tumeur, préserver le pronostic fonctionnelle ainsi que le pronostic vital en assurant une exérèse carcinologiquement satisfaisante, prévenir les récurrences locales et/ou à distance par des thérapies adjuvantes. Les épithéliomas spinocellulaires prédominaient (32 cas) puis les mélanomes (18 cas, dont 2 orbitaires) Deux exentérations ont été pratiquées dans notre étude, pour une récidive locale d’un mélanome oculaire, et un rétinoblastome. Neuf pour cent des décès ont été noté dans une série de 52 patients essentiellement en rapport avec l’étiologie maligne (7). Dans notre contexte, ces différentes voies d’abord ont permis de traiter ces tumeurs avec de bons résultats esthétiques et peu de morbidité, trois de nos malades (9,6%) avaient des complications post-opératoires. Ces complications étaient représentées par la sècheresse oculaire, le déficit du regard vers le haut, le décollement de la rétine, la diplopie, et la récidive locale. Celle-ci a concerné un cas de mélanome oculaire. La prévention des lésions infectieuses est primordiale. CONCLUSION Les TO sont multiples et rares. L’exophtalmie est le signe clinique majeur et commun de tous les patients porteurs d’un processus orbitaire. L’imagerie (TDM et IRM) permet de localiser la tumeur, et l’histologie permet de la typer. Selon leur siège, leur étendue, leur type histologique la prise en charge est différente. Elle associe la chirurgie, la radiothérapie, et la chimiothérapie. Parfois, il s’agira d’une abstention thérapeutique. L’abord neurochirurgical est le garant d’une meilleure exploration avec un objectif d’exérèse tumorale la plus complète.  Figure 1  Figure 2  Figure 3 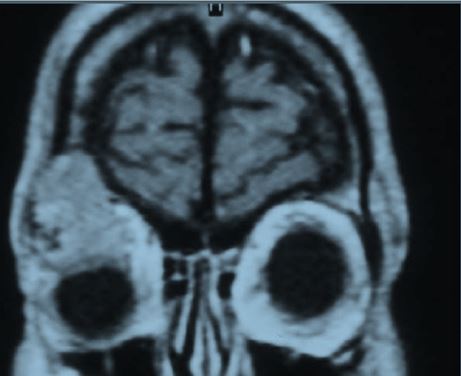 Figure 4 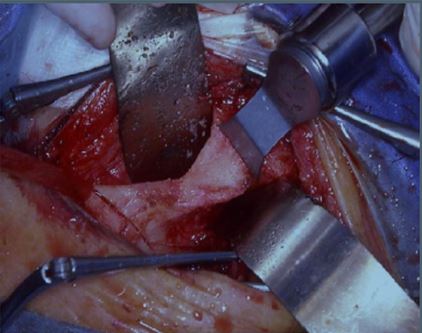 Figure 5 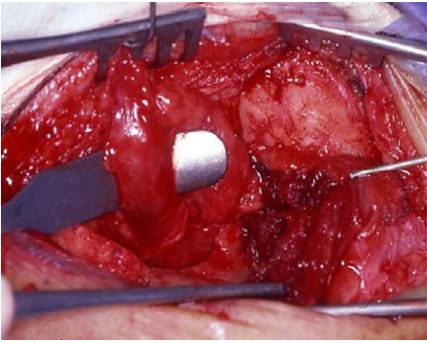 Figure 6
ABSTRACT Background and purpose: Worldwide, stroke is the second most common leading cause of death and also one of the leading causes of disability. In the last decades, more studies have focused on ischemic stroke. This study focused on intracerebral haemorrhage which is a common subtype of stroke. Method: This is a -ten year retrospective study of all autopsies with cases of intracerebral haemorrhage following hypertension as cause of death. The age, sex, anatomical location of the bleeding and any ventricular extension were extracted from the autopsy register. The data were analysed using the statistical package for social science (SPSS) Software version 18. Results: There were 397 cases of intracerebral haemorrhage with age ranging from 16 and 85 years. The mean, mode and median ages were 50.45±12.47, 50 and 50 years respectively. There were 272 (68.5%) males and 125 (31.5%) females with a male to female ratio of 2.2:1. Age group 41 – 50 years has the highest prevalence, while the least value (5.3%) was seen for the 70 years and above. The most common site of bleeding was the cerebral hemisphere with 88% having ventricular extensions. This study revealed that hemispheric haemorrhage occurred in approximately three out of every four haemorrhagic strokes. Conclusion: Hemispheric haemorrhage is the most common site of bleeding in this study, the majority of which are complicated by ventricular extension. The male sex is twice more affected than the females and the highest occurrence is seen in males in the 41-50 years age group. Keywords: cerebrum, bleeding, brainstem, cerebellum, intracerebral haemorrhage, ventricle INTRODUCTION Spontaneous non-traumatic intracerebral haemorrhage is bleeding into the parenchyma of the brain with occasional extension into the ventricles and rarely into the subarachnoid space [22]. It commonly occurs in the lobes of cerebral hemispheres, basal ganglia, thalamus, brain stem and cerebellum.[17] If the haemorrhage occurs in the basal ganglia and thalamus, this is designated ganglionic haemorrhage while those that occur in the cerebral lobes are called lobar haemorrhages [24]. This haemorrhage could also either be primary or secondary depending on the underlying cause of the bleeding. Those due to hypertension following damage to the small vessels or amyloid angiopathy are referred to as primary haemorrhage while other causes such as tumour, defective coagulation or arterio-venous malformations are referred to as secondary intracerebral haemorrhage [11] Globally, the incidence of intracerebral haemorrhage varies from 10 to 20 cases per 100,000 population and increases with age as previously reported by various studies. [4,12,13]. This incidence is however, higher in Blacks (up to 50 per 100,000) and is twice the incidence in Whites.[23] The haemorrhage occurs in middle age to late adult life with peak incidence at about the age of 60 years [24]. Other studies have also revealed it to be more common in men than women especially those older than 55 years [13,26]. It is a clinically significant cause of morbidity and mortality. In the light of the aforementioned and considering the fact that there is paucity of autopsy studies on this subject especially in Africa. The aim of this study is to examine the epidemiological and morphological features in cases of spontaneous non- traumatic intracerebral haemorrhage secondary to hypertension at post mortem examination. MATERIALS AND METHODS This is a -ten year (January 2006 to December 2015) observational retrospective study of all autopsy cases of intracerebral haemorrhage following hypertension seen in the Department of Pathology and Forensic Medicine, Lagos State University Teaching Hospital, Ikeja, Lagos, Nigeria. The department conducts autopsy services for the teaching hospital as well as coroner’s autopsy for the state. During post mortem examinations, the skull is opened and brain is removed in all cases. The age, sex, anatomical location of the bleeding and any ventricular extension is noted. All these were recorded in a pre-designed data collection form. The data were retrieved from the autopsy reports and analyzed using the Statistical Package for Social Science (SPSS) Software version 18. The data were presented in tables, percentiles, pie chart and bar chart. Test for significant was set at P< 0.05. RESEARCH MATERIAL Approval from the Department of Pathology and Forensic Medicine of Lagos State University Teaching Hospital, Ikeja was sought and received before the study could be done. Materials used include the autopsy register, post mortem reports, and clinical notes where applicable. STUDY POPULATION Lagos State University Teaching Hospital (LASUTH), Ikeja is one of the tertiary health care institutions located in the South Western geo-political zone of the country, serving a core population of approximately seventeen (17) million people of diverse backgrounds.[21]. All cases of intracerebral haemorrhage resulting only from hypertension were used in this study. The diagnosis of hypertension at post mortem examination was made based on the following criteria. Heart weight in excess of 300gm for females and 350gm for males; left ventricular wall thickness of more than 1.5cm taken at a point 1-2cm below the mitral valve and papillary muscle thickness of more than 1.5cm.Any other causes of ventricular hypertrophy such as aortic stenosis were excluded. It includes all ages and sex. All embalmed bodies with intracerebral haemorrhage were also included. Thirty five cases with advanced decomposition and who had subarachnoid haemorrhage from aneurysmal rupture or any other causes were excluded. Also excluded were cases of intracerebral haemorrhage not caused by hypertension such as coagulation disorders, tumours, arteriovenous malformation and illicit sympathomimetic drugs (amphetamine or cocaine overdose). RESULTS There were a total of 397 cases of ICH with evidence of hypertensive heart disease. The age range in this study was 16 to 85 years. The mean, mode and median ages were 50.45±12.47, 50 and 50 years respectively. There were 272 (68.5%) males and 125 (31.5%) females with a male to female ratio of approximately 2.2:1. See Table 1. Age classification was done in decades starting from below 30 years to 70 years and above age groups. The highest value of 116 (29.2%) was seen in age groups 41 – 50 years, this was closely followed by 51 – 60 years age groups representing 109 (27.5%) while the least value of 21 (5.3%) was seen for the 70 years and above age groups. The most common site of bleeding was the cerebral hemisphere which accounted for 292 (73.6%). The second most affected part of the brain was in the pontine region representing 76 (19.1%) while cerebellar haemorrhage accounted for 29 (7.3%). This study revealed that hemispheric haemorrhage occurred in approximately three out of every four haemorrhagic stroke. (Table 1). Among those post mortem with bleedings into cerebral hemisphere a total of 88% had ventricular extension. See Figure 1. Table 4 also revealed P value of 0.389, this implies that the hemorrhage affected all the parts of the brain equally across the age groups. DISCUSSION Worldwide, stroke is the second most common leading cause of death and also one of the leading causes of disability [7,19]. That its burden will most likely increase in developing countries has been corroborated by previous works [1, 27]. In the last decades, a lot of progress has been achieved in the etiology and management of stroke although; most studies have focused on ischemic stroke [14]. This study focused on intracerebral haemorrhage which is a common subtypes of stroke and constitutes 10-20% of all strokes globally and 20-30 % in Africa [6, 8]. To the best of our knowledge there is no other post mortem series on stroke secondary to hypertension published from Nigeria and the rest of Africa. The available data on intracerebral haemorrhage has been deduced from African American and the Caribbean.[9,16,3] Our study revealed that intracerebral haemorrhage from hypertension occurred twice as common in males than females. The highest incidence also occurred in the 41-50 year age group. These two findings are consistent with a clinico-pathological studies on cerebrovascular accidents done in Ibadan, Western Nigeria by Osuntokun et al [20]. In their study, the peak incidence was in the age group 40-49 years with male to female ratio of 1.7 to 1. It is also supports and consistent with the findings of Ezeala- Adikaibe in South Eastern Nigeria [5] in which ICH was diagnosed from all the CT scan over a period of 11 years. Their study revealed male to female ratio of 2 to 1 with a mean age of 58.8 years; lobar and deep cerebral haemorrhage peaked at 16-39 and 40-49 years respectively. It is also worthy of emphasis, that peak age of incidence of ICH in our study was 41-50 years. This is in agreements with the study in Nigeria by Ezeala- Adikaibe in South Eastern Nigeria [5].This revelation is not surprising considering the sedentary habits, drug use, alcohol consumption, smoking and eating habits of people in this age groups who are The glaring predominance of hemispheric haemorrhage as the overall most common ICH sites in our study is corroborated by previous works in Mexico by Ruiz-Sandoval et al [25], USA[9], France [13]Sweden [18], Japan [15], Finland [10] and Australia.[2]. However, this is in contrast with the findings in a large population-based study in Japan [15] where it accounted for only 15%, while putamen was the most common (34%). The reason for this could be a subject for future study. In most populations [13, 9, 25, 18, 15, 10,] incidence of cerebellar haemorrhage is usually higher than pontine haemorrhage. These findings are however at variance with our results where this was the reverse except in the 41-50 and 61-70 age groups. Again, our work was an autopsy based study while others were clinically based suggesting that more deaths resulted from pontine haemorrhage. This finding could be due to high incidence of hypertension in the former and the likelihood of high occurrence of amyloid angiopathy in the latter groups. An interesting finding is the very small percentage of ventricular extension reported in a previous study in Eastern Nigeria.[5]. This is in contrast to our study which revealed a predominant ventricular extension. The previous study made their diagnoses on CT scan, there was a possibility of missing out some of the ventricular extensions especially if enough slices were not made. In addition, many patients may likely survive if the ventricular extension is minimal, while majority will be fatal if the extension is massive. The latter could have accounted for the predominant percentage since it was an autopsy based study CONCLUSION Hemispheric haemorrhage (Deep and Lobar haemorrhage) most of which are complicated by ventricular extensions is the commonest site of bleeding in this study. Frequency in males is twice that of the females while the highest occurrence is seen in males in the 41-50 years age group.This study revealed that hemispheric haemorrhage occurred in approximately three out of every four haemorrhagic strokes. Financial Support and Sponsorship. Nil Conflicts of interest There are no conflicts of interest Author’s contribution SSS is a Lecturer and Consultant Pathologist who was responsible for the conceptualization, design of the study and did the literature search. FFA is a Senior Lecturer who contributed to the literature search and did the critical review of the article for intellectual content. OOO and SDA are consultant pathologists who analyzed the data while WOO is a senior registrar who collected the data. All authors read through the draft and approved for publication. Table 1. Table showing the gender, age and site of bleeding distribution (n=397)
Table 2: Table showing the distribution of sex with age groups. (n=397)
P= 0.289 Table 3: Table showing sex distribution with site of bleeding. (n=397)
P= 0.771 Table 4: Table showing age distribution with site of bleeding. (n=397)
p=0.389 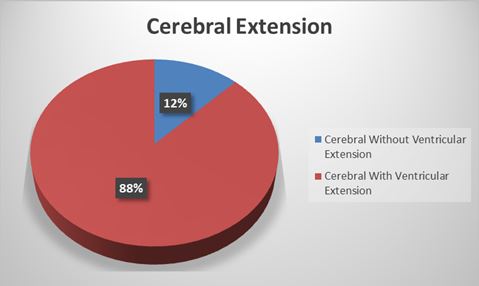 Figure 1
Articles récents
Commentaires récents
Archives
CatégoriesMéta |
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647





















